New research found low in vitro efficacy of common antimicrobial agents used to treat methicillin-resistant or sensitive Staphylococcus aureus (MRSA and MSSA) infections of the lacrimal system. Many of the antibiotics examined—mainly β-lactams and fluoroquinolones—demonstrated high rates of resistance, much greater than those of trimethoprim/sulfamethoxazole (TMP/SXT) and gentamicin, prompting the study authors to recommend the latter approach for systemic and topical single-agent treatments.
The study, conducted over 10 years at the Bascom Palmer Eye Institute at the University of Miami, assessed the microbial characteristics and management of Staphylococcus aureus by retrospectively reviewing culture-positive S. aureus isolates from lacrimal system samples. Other clinical characteristics analyzed included recent history of ocular surgery, presence of lacrimal biomaterial implant and antimicrobial regimen.
A total of 116 S. aureus isolates were identified in 116 patients. Of these, 31 patients (27.4%) had recently undergone ocular procedures, while 22 (19.5%) had received lacrimal intubation. The first line of treatment for 50 patients (44.2%) involved a combination of oral and topical antibiotics, the most frequently prescribed being β-lactams (38.9%) and polymyxin B/trimethoprim (31.0%).
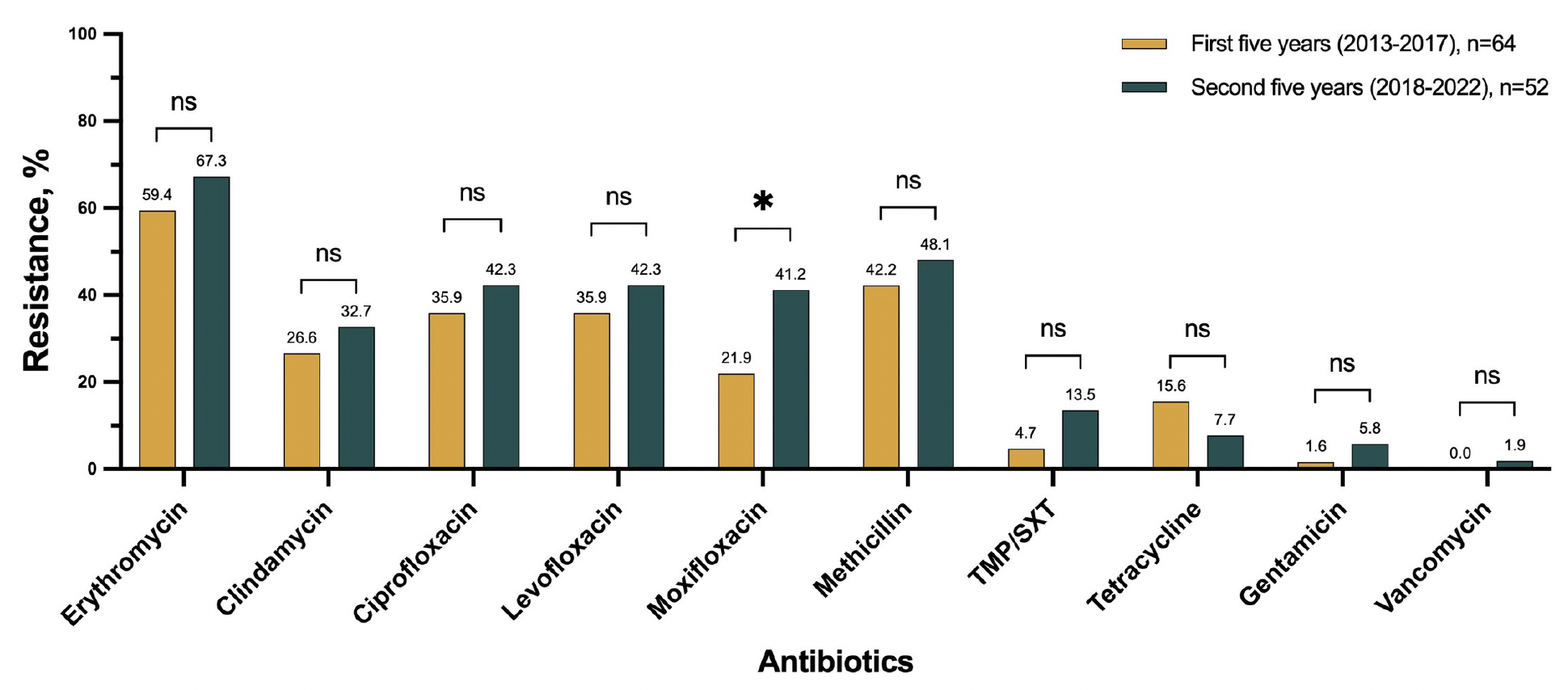 |
| This study advises against the use of single-agent therapy with antibiotics such as β-lactams and fluoroquinolones for patients with MRSA or MSSA infections of the lacrimal system. Instead, it recommends “using TMP/SXT and doxycycline for systemic treatment, along with gentamicin for topical application.” Photo: Bineshfar N, et al. PLoS One. 2024;19(11):e03143661. Click image to enlarge. |
In roughly one in five patients (20.5%), the antibiotic regimen was modified at least once due to a lack of effectiveness. For patients with positive cultures from the lacrimal system, 37.3% required surgical intervention as part of their treatment.
Among all identified isolates, 44.8% were classified as MRSA. Regarding fluoroquinolone resistance, ciprofloxacin and moxifloxacin exhibited rates of 38.8% and 30.4%, respectively, with significantly higher resistance observed in MRSA strains. Conversely, resistance rates were much lower for TMP/SXT (8.6%) and gentamicin (3.4%).
Considering these findings, the study authors stated in their paper that “single-agent therapy with these antibiotics should be avoided.” As an alternative, they noted, “We recommend using TMP/SXT and doxycycline for systemic treatment, along with gentamicin for topical application.”
Additionally, the authors point out that most patients with MRSA didn’t have classical risk factors for the infection, and only 11.1% had lacrimal biomaterials. Conversely, patients with MSSA had significantly higher rates of ocular surgery history and lacrimal intubation.
“Given the lack of evident risk factors for MRSA infection in some patients,” the authors concluded, “[eyecare providers] should always consider MRSA as an etiology for lacrimal apparatus infections, even in the absence of any risk factors.”
| Click here for journal source. |
Bineshfar N, Clauss KD, Lee WW, Miller D. Microbiology and management of Staphylococcus aureus lacrimal system infections: a 10-year retrospective study. PLoS One. 2024;19(11):e03143661. |