|
The intriguing topic of imaging in malpractice allegations was first mentioned in the December 2023 You Be the Judge article entitled “Maybe Too Thin?” This case was about a fashion model on Plaquenil (hydroxychloroquine, Sanofi) for rheumatoid arthritis for only about 30 months who unexpectedly developed toxic maculopathy in both eyes. The first eyecare clinician to evaluate the patient when she was on Plaquenil for 15 months appropriately performed a comprehensive exam including OCT, which was normal and interpreted as such. About a year later, the patient was evaluated by a different eyecare clinician in a different practice who also appropriately performed a comprehensive exam including OCT.
When malpractice allegations ensued, a review of all the records, emphasizing the all-important spectral-domain OCT (SD-OCT) findings, revealed that only the SD-OCT performed by the second eye clinician, which was interpreted as normal, was clearly abnormal and characteristic of Plaquenil-induced toxic maculopathy OU.
Hence, the normal OCT on the first visit shielded the first clinician from successful malpractice allegations but provided irrefutable evidence that the second clinician deviated from the existing standard of care by misinterpreting the SD-OCT, which resulted in irreversible loss of vision and culpability of malpractice. We can conclude that imaging (the OCT) was a friend for the first doc and a foe for the second.
In this new case below, ultra-widefield (UWF) fundus imaging clearly documents a misdiagnosis that recently resulted in a large settlement for the plaintiff.
 |
|
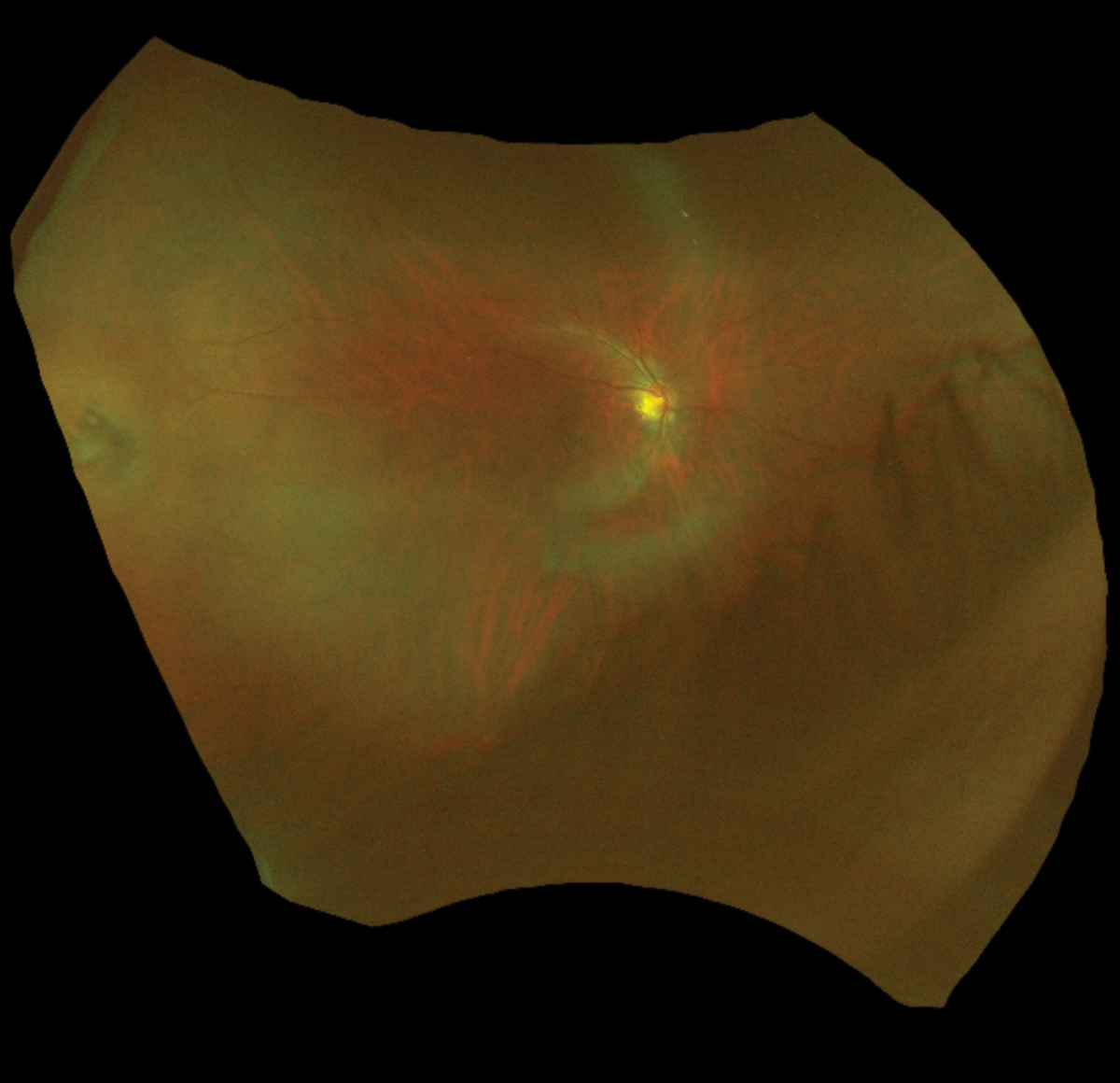
Lesion at nine o’clock was diagnosed as CHRPE on this visit and subsequent visits. Click image to enlarge. |
Case
A 50-year-old myopic man presented for routine care including a new spectacle prescription and updated contact lenses. The health history and previous eye history were unremarkable. The 7D myope was evaluated by the same ophthalmic clinician on five occasions over a six-year period. UWF Optos images were obtained on each visit. The patient never complained of flashes but mentioned occasional floaters in the right eye during the last two visits. A posterior vitreal detachment was noted by the eye clinician in the right eye, and a possible risk of retinal detachment was explained to the patient. The patient never complained of field loss on any of these visits.
On the first visit, the eye doc diagnosed a CHRPE (congenital hypertrophy of the retinal pigment epithelium) lesion in the periphery of the right eye. The location of the lesion was not noted, and a drawing or sketch of the lesion was not included. With minor changes in the prescription, the patient’s visual acuity (VA) was improved to 20/20 in each eye on all five visits. The CHRPE lesion was noted on all subsequent examinations. The patient was dilated on three of the five visits and refused dilation on the other two. Several months after the last visit, the patient began complaining of decreased vision in the right eye, was referred to a retinal specialist and was diagnosed with an inferior retinal detachment OD. The retinal specialist noted that “the primary break was temporal.” The retinologist did not identify any CHRPE lesions in either eye.
You Be the Judge
Given the facts presented thus far, consider the following questions:
- Was the lesion the primary eye clinician imaged and documented on several occasions a CHRPE?
- Was the temporal retinal break that eventually enlarged to a retinal detachment misdiagnosed as a CHRPE lesion?
- If the lesion was correctly diagnosed as a retinal break years earlier, would the outcome be different?
- Can experts for the eye clinician present any meaningful arguments for the defense?
- Were the UWF images in this case friend or foe for the primary eye clinician?
Our Opinion
One of us (JS) was requested to review all the records with emphasis on the multiple UWF images. I concluded that the temporal retinal break that was imaged with the UWF device was repeatedly misdiagnosed by the eye clinician as a CHRPE lesion. The delay in diagnosis and subsequent delay in treatment resulted in the need for a scleral buckle and pars plana vitrectomy. Although the combined procedure was successful from a surgical point of view, this essential intervention then resulted in a cataract in the right eye, which required removal. A secondary cataract, a posterior capsular opacification, developed, which will require treatment. The patient also developed cystoid macula edema (CME) as a result of the combined surgical intervention and an epiretinal membrane. The CME has required a combination of steroid drops, perhaps for a prolonged period of time, which increases the risk of infection in the right eye and other side effects. I opined that the retinal break could have been diagnosed on the first visit and treated successfully with cryotherapy or laser six years earlier.
I asked my new associate, DD, to review the images, as I have done in previous cases. Dr. Doscas immediately diagnosed the lesion as a retinal tear in the temporal retina of the right eye.
 |
|
UWF image taken the day the detachment was diagnosed by the retina surgeon. The lesion at nine o’clock was diagnosed as a retinal tear that resulted in the retinal detachment. Click image to enlarge. |
The Defense
Two highly respected MD experts with impressive credentials and publications reviewed the case files and reached the following conclusions. Both acknowledged that the lesion documented with UWF Optos images was not a CHRPE but a retinal break and, hence, misdiagnosed by the primary eyecare clinician. One of these experts stated, “CHRPE is a benign condition, showing lesions with flat, hyperpigmentation. CHRPE is an uncommon but not rare retinal condition with a prevalence of about 1% to 2%. I believe that Dr. X incorrectly diagnosed CHRPE due to the presence of pigmentation seen around the retinal tear.”
This expert added, “It should be noted that asymptomatic retinal breaks such as seen in this case have only a 5% chance of developing retinal detachment […] Had the patient been referred out to a retinal specialist, it is entirely possible that no treatment would have been offered, particularly since the tear was already partially self-demarcated (i.e., pigment was present around some of the tear). Had laser treatment and or cryotherapy been opted for, there is roughly a 10% failure rate due to development of recurrent retinal tears. There is a roughly 3% to 10% chance of developing epiretinal membrane after either of these treatments.”
I (JS) have no substantive disagreement with either physician in their summary of the surgeries and care rendered by others prior to and subsequent to these surgeries, save perhaps for the care rendered by the defendant, which both experts appear to have avoided. My opinion remains that the failure to diagnose the retinal tear initially and over several years subsequently resulted in the need for these surgeries. If the primary eyecare clinician met the standard of care and did not misdiagnose the retinal tear as a CHRPE lesion, the tear could have been treated successfully with laser or cryo and avoided both surgeries.
Fortunately, the patient is left with normal near central vision but does demonstrate loss of perhaps 6% of his macula vision, as documented with the Humphrey Visual Field Analyzer. There remains, and will forever, superotemporal peripheral vision loss in the right eye. There is also metamorphopsia, or distortion of vision where straight lines appear to bend or curve. This annoying distortion will likely last forever. The macular pucker, or epiretinal membrane scarring, is a result of the retinal detachment surgery, which could have been avoided if the correct diagnosis was arrrived at initially and treated with laser or cryo.
The agony, pain, suffering and other stress-related issues associated with the surgery, as well as costs not covered by insurance, including a $2,000 toric intraocular lens, all relate to the wrong diagnosis.
Follow-up
In a Midwestern state where this all occurred, both sides agreed to mediation rather than going to trial. We have no experience with mediation in malpractice cases and cannot comment on how this approach works. The bottom line in this case was that the patient was awarded an amount well into six figures.
Hence, the UWF images were not a friend but a foe to this primary eyecare clinician. The three authors are all fans of UWF imaging, but the images must be correctly interpreted to avoid such disasters.
Dr. Doscas graduated from SUNY College of Optometry in 2023. She completed her residency training in primary care optometry and ocular disease at VA Hudson Valley and is currently employed at a private practice in White Plains, NY.
| NOTE: This article is one of a series based on actual lawsuits in which the author served as an expert witness or rendered an expert opinion. These cases are factual, but some details have been altered to preserve confidentiality. The article represents the authors’ opinion of acceptable standards of care and do not give legal or medical advice. Laws, standards and the outcome of cases can vary from place to place. Others’ opinions may differ; we welcome yours. |
Dr. Sherman is a Distinguished Teaching Professor at the SUNY State College of Optometry and editor-in-chief of Retina Revealed at www.retinarevealed.com. During his 52 years at SUNY, Dr. Sherman has published about 750 various manuscripts. He has also served as an expert witness in 400 malpractice cases, approximately equally split between plaintiff and defendant. Dr. Sherman has received support for Retina Revealed from Carl Zeiss Meditec, MacuHealth and Konan.
Dr. Bass is a Distinguished Teaching Professor at the SUNY College of Optometry and is an attending in the Retina Clinic of the University Eye Center. She has served as an expert witness in a significant number of malpractice cases, the majority in support of the defendant. She serves as a consultant for ProQR Therapeutics.