|
Q:
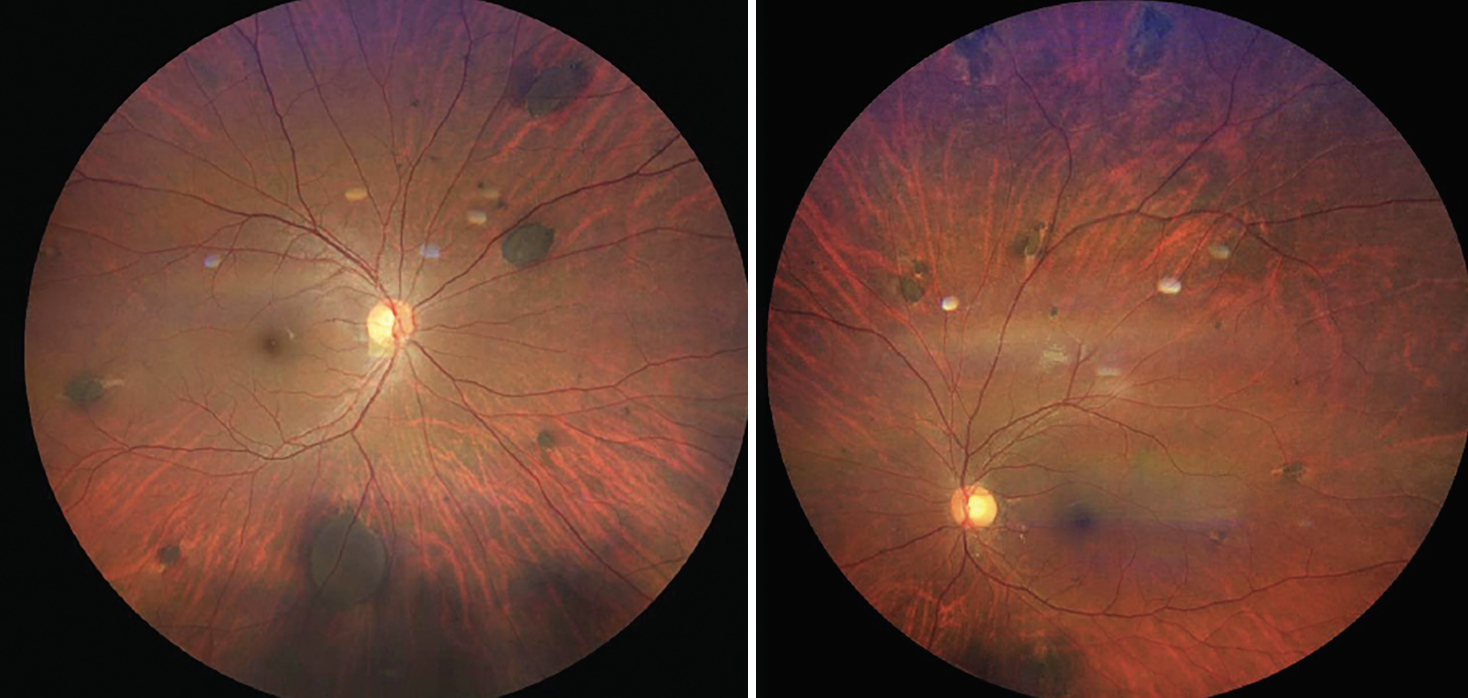
A 40-year-old presented to me with multiple atypical congenital hypertrophy of the retinal pigment epithelium (CHRPE) lesions and no systemic diagnosis. I know that CHRPEs can be a benign finding in most patients, but when should I be concerned?
CHRPEs can be idiopathic or be associated with Gardner’s syndrome, a variant of familial adenomatous polyposis (FAP). “The goal is to recognize the unique presentation of these CHRPEs and know when to facilitate appropriate testing and referral,” says Alek Karthikeyan, OD, of Rochester, NY. “These patients are at high risk of early death from colon cancer.”
What to Look For?
There are three main variations of the condition, the first and most common being solitary CHRPE. This lesion represents hypertrophy and hyperplasia of the RPE cells and is typically unilateral and not associated with any systemic conditions.1 The second are grouped CHRPE, also known as “bear tracks.” These lesions represent an increase in the pigmentation within the melanin granules of the RPE cells and are typically unilateral, multifocal and confined to a single quadrant of the retina.1 “There is a common misconception that bear tracks are associated with Gardner’s; however, these lesions have no systemic associations and are benign in nature,” Dr. Karthikeyan says.
The last and least common presentation are CHRPE associated with FAP. These lesions are bilateral, multifocal and extend into different quadrants. They often have a “pisciform” appearance with irregular depigmented borders, as seen in this patient’s fundus. These CHRPE are the earliest and most common extracolonic manifestations of FAP.2 The presence of four or more CHRPE is highly specific for this systemic pathology.
 |
|
A patient with Gardner’s syndrome. Click image to enlarge. |
Next Steps
When these suspicious lesions are identified on exam, Dr. Karthikeyan says it’s imperative to do a deep dive in the patient’s family history and review of systems for any gastrointestinal symptoms. Upon further questioning, he identified that the patient’s father and brother both died of cancer. Additionally, the patient also reported routine hematochezia (blood in stool). All these findings lined up with a slam dunk diagnosis. This patient hadn’t seen a doctor in a long time, so an emergent referral was made to a primary care provider within our health system. He was quickly referred to a gastroenterologist for a colonoscopy and related testing, but was lost to follow up.
The pathologic sign of FAP is the development of hundreds to thousands of polyps within the colon and rectum. These will inevitably transform into colon cancer if left untreated (7% risk by age 21, increasing to 87% by age 45 and then 93% by age 50).3 Gardner’s syndrome is a variant of FAP, where there are additional extracolonic manifestations, such as CHRPE, desmoid tumors, osteomas and dental abnormalities, to name a few. When 30 or more polyps are detected, removal of the colon and rectum may be recommended. According to Dr. Karthikeyan, the ultimate goal is to prevent development of colon cancer and associated malignancies.
ODs play a critical role in detecting atypical CHRPEs early in patients with Gardner’s syndrome and setting a precedent in addressing this disease process. Trust your gut when you see these lesions, and facilitate appropriate referrals to potentially add years to your patients’ lives.
Dr. Ajamian is board certified by the American Board of Optometry and serves as Center Director of Omni Eye Services of Atlanta. He is president of the Georgia State Board of Optometry and general CE chairman of SECO International. He has no financial interests to disclose.
1. Ireland AC, Rodman J. Congenital hypertrophy of retinal pigment epithelium. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. www.ncbi.nlm.nih.gov/books/NBK576424/. Last updated May 15, 2024. Accessed September 1, 2024. 2. Bonnet LA, Conway RM, Lim LA. Congenital hypertrophy of the retinal pigment epithelium (CHRPE) as a screening marker for familial adenomatous polyposis (FAP): systematic literature review and screening recommendations. Clin Ophthalmol. 2022;16:765-74. 3. Yen T, Stanich PP, Axell L, et al. APC-Associated polyposis conditions. In: Adam MP, Feldman J, Mirzaa GM, et al., eds. GeneReviews [Internet]. Seattle (WA): University of Washington, Seattle. www.ncbi.nlm.nih.gov/books/NBK1345/. Last updated May 12, 2022. Accessed September 1, 2024. |