|
A 57-year-old Black man presented to the office with a chief complaint of blurry vision OU of one month’s duration. He was interested in a new spectacle prescription. He had no prior history of trauma or pain. His systemic and ocular histories were unremarkable. He denied allergies of any kind.
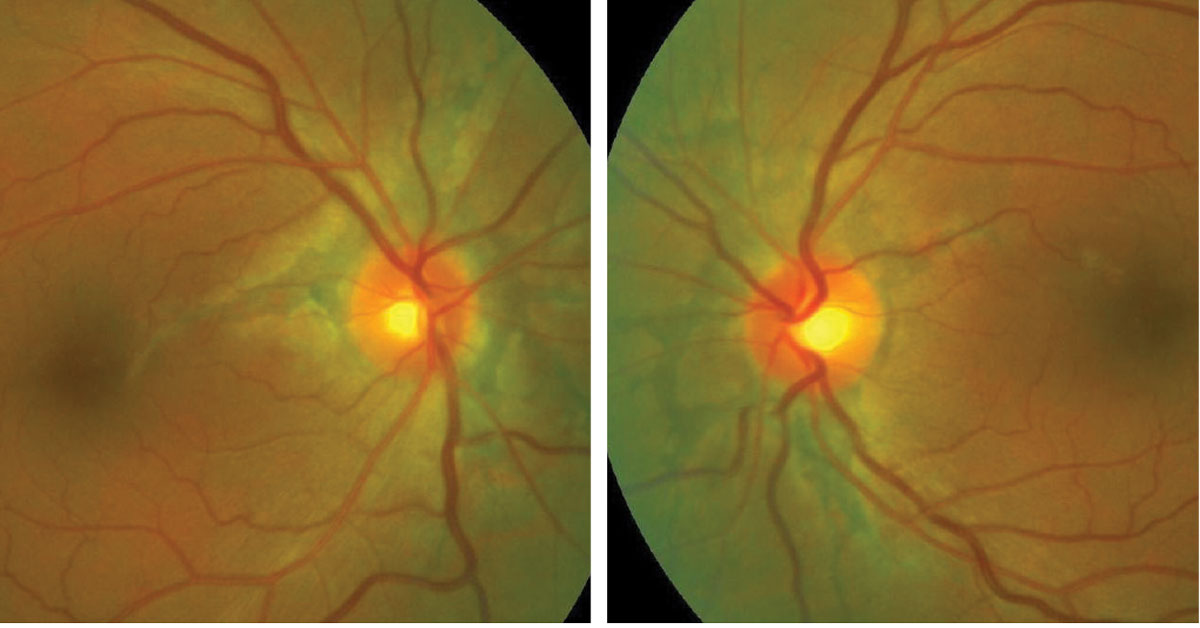
His best-corrected acuities were 20/20 OD and 20/20 OS at distance and near. External exam was normal and there was no afferent pupil defect. Refraction was negligibly different with an excellent visual response. His anterior segment structures were normal with Goldmann tonometry measuring 17mm Hg OU. Cup/disc ratios were 0.2 OD and 0.25 OS. The dilated fundus findings were normal peripherally, with the pertinent findings surrounding both nerves demonstrated in the photographs.
Additional studies might include color photography of both nerves, automated perimetry to rule out functional loss and five-line raster of the area about both nerves to rule out choroidal neovascularization. Additional history might be requested to rule out collagen vascular disease such as pseudoxanthoma elasticum and Ehlers-Danlos syndrome, Paget’s disease and sickle cell anemia. Lab work and correspondence with the GP was completed.
 |
|
Fundus appearance of the patient's right and left eyes. Click image to enlarge. |
Disc Anomaly
The relevant clinical finding in this issue is angioid streaks (AS) OU. Angioid streaks appear as jagged, irregular reddish-brown radiations that emanate from the optic disc. These represent dystrophic calcification of Bruch’s membrane.1-15 They may occur idiopathically, as a result of age-related or genetic processes, in association with cardiac anomalies, secondary to hemoglobinopathies such as sickle cell anemia, or secondary to diseases affecting collagen or connective tissue such as pseudoxanthoma elasticum, Paget disease and Ehlers-Danlos syndrome.1-8
Since angioid streaks are a finding and not a diagnosis, there is no epidemiologic data per se; that is, they occur with some frequency in association with selected systemic conditions.1-15
The physical expression of angioid streaks is related to lines of force created by the extraocular muscles that surround the eye about the optic nerve.7-9 The discoloration of the affected Bruch’s membrane is related to degeneration of its multiple elastic layers along with deposition of calcium, magnesium and iron salts as a result of the disrupted metabolism, produced in part by the systemic disease that triggered the process.7-9
The ultimate deleterious outcome of these subretinal phenomena is the formation of choroidal neovascular membrane (CNV) with or without catastrophic bleeding and disciform scarring.1-13
CNV has the potential to produce vision-threatening subretinal fluid, exudate and blood.1-13 The incidence of CNV in angioid streaks has been documented to be as high as 86% with bilateral involvement seen in up to 71% cases.1 Typically, the CNV produced in angioid streaks is type II (majority of the membrane exhibiting breakthrough, existing above the RPE; however, type I CNV (below the RPE) is also plausible.1,8,12-15 The wider and longer the AS, the greater the risk of CNV development.8,10
If CNV is suspected, referral to retinology is indicated for OCT or OCT angiography, as well as for possible intravenous fluorescein angiography. If CNV is discovered, combinations of laser photocoagulation and anti-VEGF injections may be indicated.8,12-15
The natural course of AS ranges from age-related degeneration with no vision-affecting outcomes to CNV formation with bleeding, disciform macular scarring, helicoid peripapillary atrophy and diffuse choroidal sclerosis, resulting in obscuration of the streaks themselves.8-14
Correspondence was sent to this patient’s general healthcare practitioner so that a proper laboratory work-up could be completed for the commonly associated systemic diseases. The work-up results were negative. To date, there have been no new pathologic changes; he is monitored with dilated examinations at six- to eight-month intervals and at home with an Amsler grid.
Dr. Gurwood is a professor of clinical sciences at The Eye Institute of the Pennsylvania College of Optometry at Salus University. He is a co-chief of Primary Care Suite 3. He is attending medical staff in the department of ophthalmology at Albert Einstein Medical Center, Philadelphia. He has no financial interests to disclose.
1. Chatziralli I, Saitakis G, Dimitriou E, et al. Angioid streaks: a comprehensive review from pathophysiology to treatment. Retina. 2019;39(1):1-11. 2. Matonti F, Conrath J. Angioid streaks. J Fr Ophtalmol. 2012;35(10):838-45. 3. Germain DP. Pseudoxanthoma elasticum. Orphanet J Rare Dis. 2017;12(1):85. 4. Takkar B, Rathi A, Venkatesh P, Kumar A. Giant idiopathic angioid streaks. J Ophthalmic Vis Res. 2020;15(2):240-5. 5. Asano S, Nakajima K, Kure K, et al. Corneal biomechanical properties are associated with the activity and prognosis of angioid streaks. Sci Rep. 2018;8(1):8130. 6. Cebeci Z, Bayraktar S, Oray M, Kir N. Silent polypoidal choroidal vasculopathy in a patient with angioid streaks. Arq Bras Oftalmol. 2016;79(3):200-1. 7. Marchese A, Parravano M, Rabiolo A, et al. Optical coherence tomography analysis of evolution of Bruch's membrane features in angioid streaks. Eye (Lond). 2017;31(11):1600-5. 8. Tripathy K, Quint JM. Angioid streaks. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2020. 9. Klein BA. Angioid streaks: a clinical and histopathologic study. Am J Ophthalmol. 1947;30(8):955-68. 10. Mansour AM, Shields JA, Annesley WH, et al. Macular degeneration in angioid streaks. Ophthalmologica. 1988;197(1):36-41. 11. Mansour AM, Ansari NH, Shields JA, Annesley WH, Cronin CM, Stock EL. Evolution of angioid streaks. Ophthalmologica. 1993;207(2):57-61. 12. Patel R, Wang J, Campbell JP, et al. Classification of choroidal neovascularization using projection-resolved optical coherence tomographic angiography. Invest Ophthalmol Vis Sci. 2018;59(10):4285-91. 13. Chapron T, Mimoun G, Miere A, et al. Optical coherence tomography angiography features of choroidal neovascularization secondary to angioid streaks. Eye (Lond). 2019;33(3):385-91. 14. Lekha T, Prasad HN, Sarwate RN, Patel M, Karthikeyan S. Intravitreal bevacizumab for choroidal neovascularization associated with angioid streaks: long-term results. Middle East Afr J Ophthalmol. 2017;24(3):136-42. 15. Mentes J, Karaca I, Sermet F. Multimodal imaging characteristics of quiescent type 1 neovascularization in an eye with angioid streaks. Am J Ophthalmol Case Rep. 2018;10:132-6. |