 |
|
The OHTS trial, spanning 20 years, reveals significant rates of visual field loss in patients at risk for glaucoma despite regular monitoring. The study highlights rapid progression in some eyes, particularly those with visual field POAG. Researchers call for more frequent testing intervals and personalized intraocular pressure (IOP) management to better detect early glaucomatous damage, emphasizing the need for tailored care based on progression rates, patient age and medical history. Photo: Brian D. Fisher, OD. Click image to enlarge. |
Over 20 years ago, the first participants were enrolled in the Ocular Hypertension Treatment Study (OHTS). This multicenter, randomized prospective trial sponsored by the National Eye Institute was designed to determine if lowering IOP can delay or prevent the development of primary open angle glaucoma (POAG). The cohort ultimately included 1,636 individuals who were followed closely through three stages of the trial through August 2022. Results of their rate of visual field (VF) loss before and after the diagnosis of POAG were revealed in a study recently published in the American Journal of Ophthalmology, showing rapid rates of VF loss in one or both eyes, despite the fact that they were involved in a clinical study.
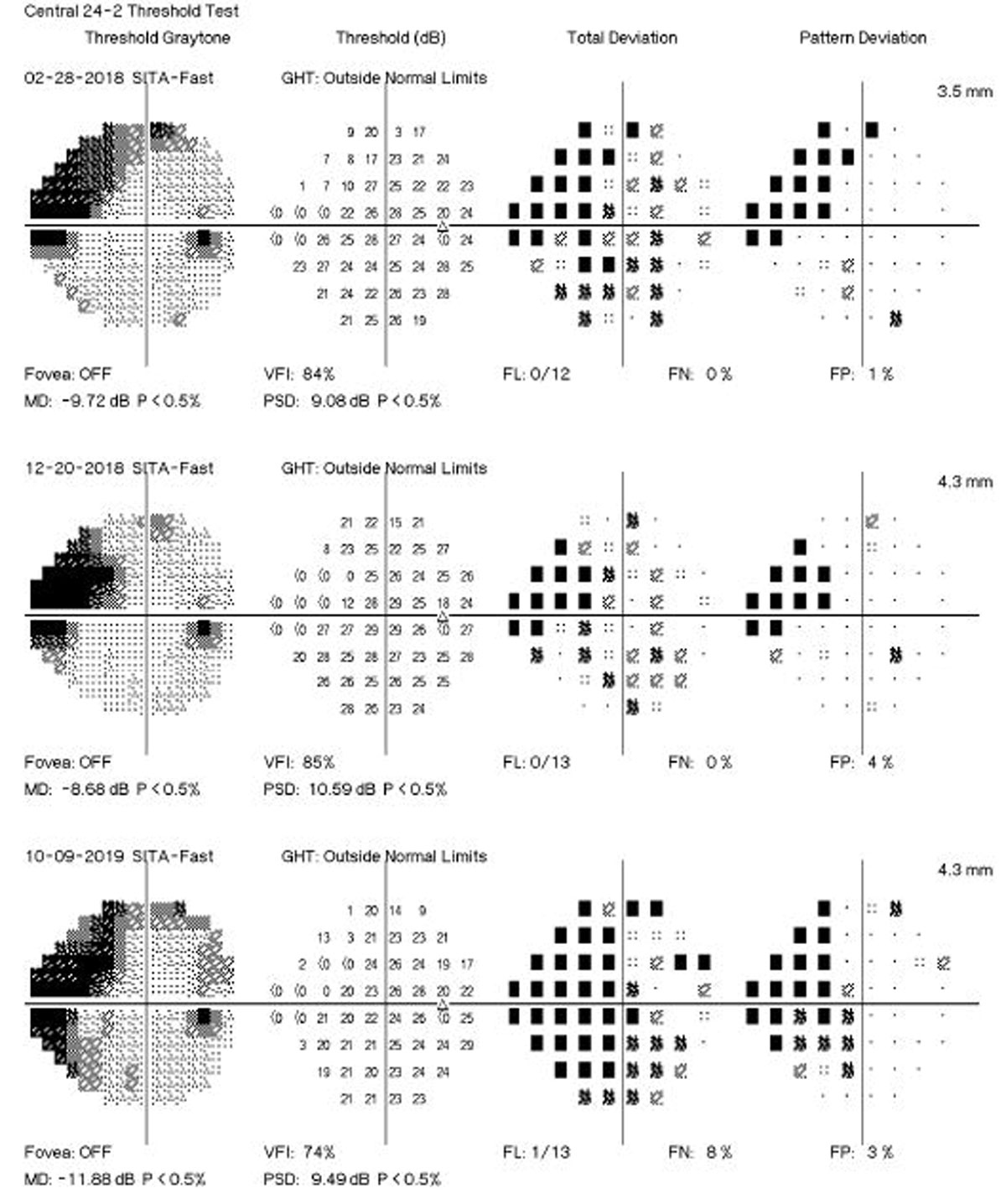
VF tests were performed every six months and stereoscopic optic disc photos were taken every 12 months during OHTS 1 and 2. These tests were repeated in OHTS 3. Slopes of mean deviation (MD) were calculated by linear regression for all eyes in OHTS 1 and 2: eyes that did not develop POAG, eyes that developed optic disc POAG only, and eyes that developed VF POAG with/without optic disc POAG. According to the results, 1,109 participants (n=2,204 eyes) did not develop POAG in either eye. The inception cohort of participants who developed POAG consists of 280 participants (369 eyes): 155 eyes of 103 participants developed only optic disc POAG and 214 eyes of 179 participants developed VF POAG with or without disc POAG.
The mean age at diagnosis of POAG was 66.4 (n= 282 participants), 56% were male, 61% were white non-Hispanic and 32% were Black non-Hispanic by self-report. The post-POAG slope was -0.40 ±0.64 dB/year for all POAG eyes (n=280 eyes), -0.19 ±0.4 dB/year for optic disc POAG only eyes (n=112 eyes), and -0.54 ±0.7 dB/year for VF POAG eyes with or without optic disc POAG (n=168 eyes). Among the VF POAG eyes, 69 (41%) had post-POAG MD slopes worse than or equal to -0.5 dB/year, 35 (21%) had slopes worse than or equal to -1.0 dB/year, and nine (5.4%) had slopes worse than or equal to -2.0 dB/year.
The study authors say the marked differences in rates of progression occurred despite all participants being volunteers in a clinical study who were examined every six months. Thirty-five eyes (21%) had post VF POAG slopes worse than or equal to -1.0 dB/year, which is considered rapid, noted the authors. Although six-month testing intervals has previously been considered optimal for detecting progression in high-risk ocular hypertensive patients, shorter testing intervals may be warranted in some patients, they speculated. “The rapid rates of VF progression in some participants in OHTS may be related to inadequate IOP goals, greater sensitivity of the optic nerve and/or retinal ganglion cells in some participants, differential adherence and persistence to medication or non–pressure dependent mechanisms of damage,” the authors wrote in the American Journal of Ophthalmology.
In eyes that developed optic disc POAG in OHTS 1 and 2 but never developed VF POAG through their last VF test, researchers reported a similar mean MD slope prior to POAG diagnosis as the eyes that never developed POAG. “However, after diagnosis of optic disc POAG, the mean slope of MD, (-0.19 dB/year) was worse than the non POAG eyes (-0.05 dB/year) but less than the VF POAG eyes (-0.54 dB/year),” they wrote. “This implies that damage to the ganglion cells was likely occurring before OHTS VF endpoints were reached.”
The strengths of this study include its large and diverse inception cohort, as well as standardized testing, diagnostic criteria, use of reading centers with masked readers and use of a masked Endpoint Committee. Authors also noted limitations, including a loss to follow up and death of participants over 20 years. This created missing data especially during OHTS 2 and 3. Change in VF was analyzed by MD only, they said. “MD is a global measure of VF sensitivity and may miss focal changes of POAG that are clinically relevant,” they wrote in the study.
Researchers say the rapid and severe VF loss in one or both eyes of participants indicated that ocular hypertensive patients require careful follow-up to detect early signs of glaucomatous damage. “At the time POAG is diagnosed, appropriate IOP goals should be set taking into consideration the rate of glaucoma progression as well as the patient’s age, medical condition, life expectancy and personal preference,” they concluded.
| Click here for journal source. |
Gordon MO et al. Visual Field Progression in the Ocular Hypertension Treatment Study. American Journal of Ophthalmology. December 6, 2024. [Epub ahead of print]. |