 |
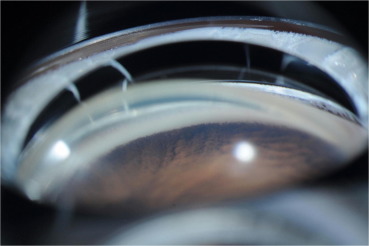
| This analysis of the IRIS registry found that children with glaucoma were more likely to receive incisional surgery if they have a higher baseline IOP or a younger age at diagnosis. The most common first-recorded procedures were angle surgery for primary congenital glaucoma, tube shunt surgery for glaucoma following cataract surgery and secondary glaucoma and SLT for juvenile open-angle glaucoma. Photo: Badawi AH, Saudi J Ophthalmol. 2019;382-8. Click image to enlarge. |
Researchers recently analyzed the nationwide IRIS (Intelligent Research in Sight) registry to evaluate treatment patterns of childhood glaucoma, a rare condition that lacks standardized clinical practice guidelines. Included were 5,017 eyes of 3,069 patients aged 18 or younger with a diagnosis code for glaucoma. Based on billing codes, 4.1% of eyes had primary congenital glaucoma (PCG), 38.1% had juvenile open-angle glaucoma (JOAG), 19.9% had glaucoma following cataract surgery (GFCS) and 32.8% had secondary glaucoma other than GFCS.
The data showed that 16.1% of affected eyes underwent glaucoma-related procedures, while 93.6% received intraocular pressure (IOP)-lowering medications, most commonly beta blockers. The procedure type varied by type of glaucoma:
- Angle surgery was the most common procedure performed for eyes with PCG.
- Tube shunt surgery was used most frequently for GFCS and secondary glaucoma.
- Laser trabeculoplasty was primarily used for JOAG, often by non-glaucoma, non-pediatric specialists.
Several factors were found to predict the likelihood of undergoing incisional surgeries. Greater baseline IOP levels (hazard ratio: 1.06 per mm Hg) were associated with a higher likelihood of surgery, as was younger age at diagnosis (especially under one year, with a hazard ratio of 6.08 compared with a diagnosis between ages 11 to 15 years). Additionally, care by non-glaucoma subspecialists was linked to a lower likelihood of incisional treatment (hazard ratio: 0.32).
While only one-sixth of patients with childhood glaucoma in this cohort underwent glaucoma-related procedures, the researchers pointed out in their paper that this sharply contrasts with a study by the Childhood Glaucoma Research Network, which found that 82.3% of eyes with PCG underwent surgery, 42.6% for JOAG and 41.7% for GFCS. One potential reason for this discrepancy, they suggested, is that “the IRIS Registry includes more data from private practices whereas previous studies have focused on academic medical centers, [and] patients who could be followed at community practices are more likely to have mild and stable disease.” Indeed, the cohort in this study had better baseline visual acuity and IOP levels than in other studies. It’s also possible that “some patients may have undergone surgery elsewhere before being captured by the IRIS Registry,” the researchers added.
Although this data provides insights into common practice patterns for childhood glaucoma, the researchers concluded that future investigations should examine the effectiveness of these management strategies to help develop accessible, standardized treatment guidelines.
| Click here for journal source. |
Fujita A, Vu DM, Aziz K. Treatment patterns of childhood glaucoma in the United States: Analysis of IRIS Registry (Intelligent Research in Sight). Am J Ophthalmol. November 29, 2024. [Epub ahead of print]. |