 |
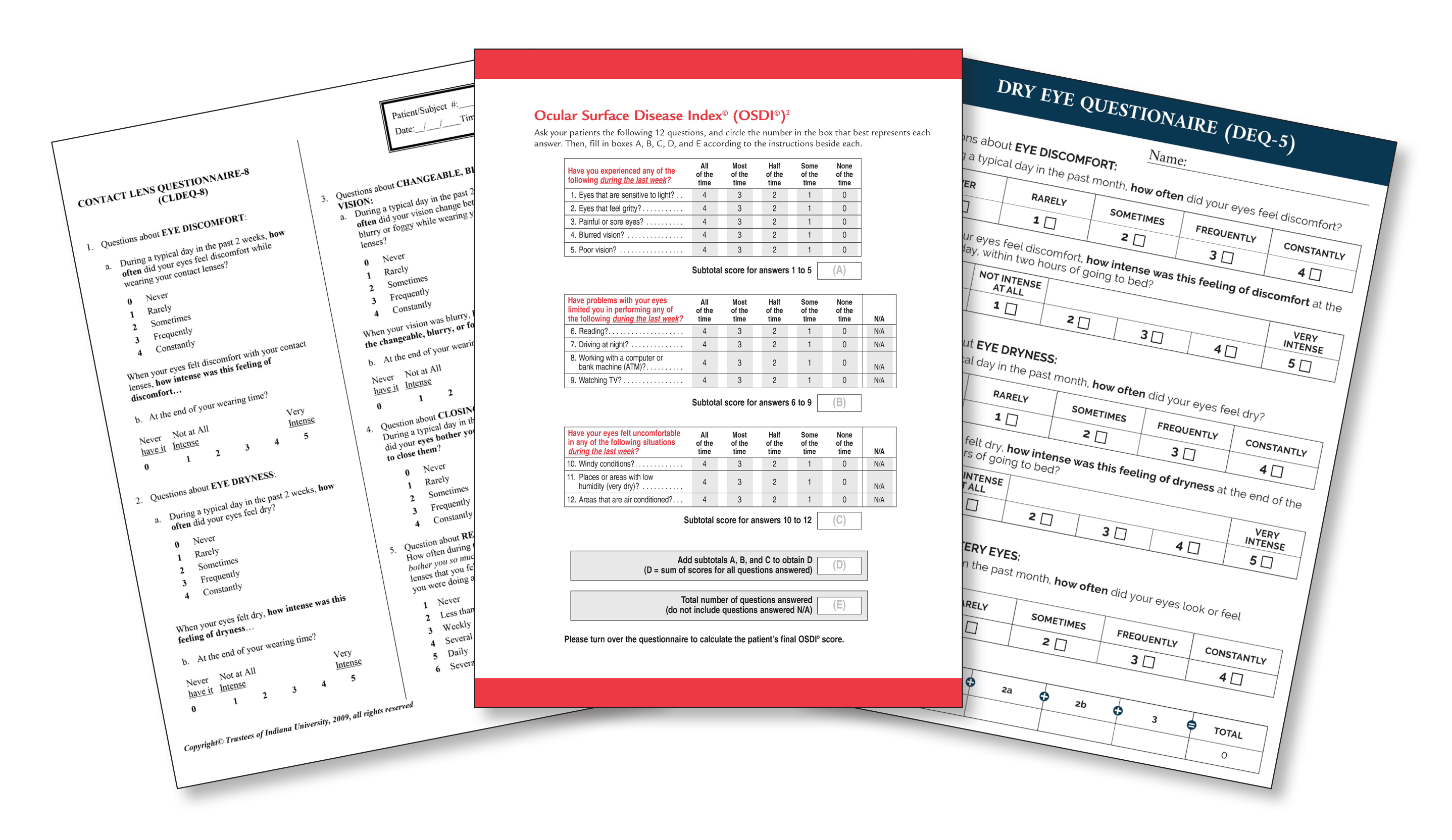
| An evaluation of 34 PROMs specific to ocular surface disease determined that the main limitations of these tools included not involving patients in their development, limited content, poor psychometric properties and multidimensionality. Click image to enlarge. |
Ocular surface diseases (OSDs) cause symptoms such as discomfort, pain and visual disturbances that can significantly affect patients' quality of life (QoL). Evaluating these subjective experiences through patient-reported outcome measures (PROMs) gives eyecare providers a fuller picture of the impact these diseases have on patients' daily lives, beyond objective clinical measurements. While dozens of PROMs have been validated for assessing QoL impacts in OSD patients, a recent systematic review highlighted several limitations in the effectiveness of these tools and proposed a new approach to PROM design.
The analysis considered a wide array of PROM instruments, including well-known ones like the Ocular Surface Disease Index (OSDI), the Dry Eye Questionnaire (DEQ), the Standard Patient Evaluation of Eye Dryness (SPEED) and many others familiar to clinicians. The work was performed at the University of New South Wales School of Optometry and Vision Science in Sydney.
“Many PROMs combine different aspects of QoL-like symptoms, activity limitations and emotional well-being into a single overall score,” notes Pawan Baral, B.Optom, lead author of the study, which recently appeared in The Ocular Surface. “While this can provide a general idea of impacts on someone,” he explains, “it often obscures details of how people are affected, [which] can make it challenging for clinicians to focus on the issues that matter most to the patients.”
To come to this conclusion, Dr. Baral and his team performed a literature search on several databases and identified 67 studies involving 34 unique PROMs used to evaluate various aspects of OSD. Of these, 16 were specific to dry eye, four to contact lenses, one to MGD, one to blepharitis, five to Sjögren Syndrome, one to computer vision, one to ocular pain and one to bone marrow transplants (used in ocular graft vs. host disease). Four generic PROMs were also assessed.
|
For an in-depth look at the clinical uses of dry eye questionnaires, see this feature with input from leading experts. |
After analyzing these studies, the researchers discovered that most PROMs had poor psychometric properties, including reliability and validity. Twenty-five out of 34 PROMs did not incorporate patient input during the development process, and 24 focused solely on measuring symptoms, omitting items related to other QoL domains (such as activity limitations and social and emotional wellbeing). Even for the nine PROMs that did assess QoL domains aside from ocular comfort and vision, the researchers argue that the multidimensional nature of these tests may introduce ambiguity and result in inaccurate assessments.
“When a multidimensional PROM is used for measurement, it may be unclear what the score actually represents, it becomes difficult to identify which domain is responsible for changes in overall score, the measurement precision may be low and it may fail to fully capture each domain nuances,” the researchers wrote in their study.
Considering these limitations, which the authors say made them unable to “recommend a single best PROM for measuring OSD-specific QoL,” they proposed an alternative approach to PROM design that could better capture the multifaceted impacts of ocular surface diseases.
“Ideally, well-designed PROMs provide separate scores for individual traits, such as a symptom score or an activity limitation score,” Dr. Baral explains. “These focused scores can allow clinicians to effectively measure the severity of the problem and make it easier to evaluate the benefits of treatment,” he argues.
Dr. Baral notes that “while PROMs are valuable for incorporating the patient perspective into care, their effective use requires careful interpretation.” The development of “more comprehensive and rigorously validated PROMs will enhance their role in managing OSD and improving patient outcomes,” he concludes.
| Click here for journal source. |
Baral P, Kumaran SE, Stapleton F, Pesudovs K. A systematic review assessing the quality of patient reported outcome measures in ocular surface disease. Ocul Surf. December 2, 2024. [Epub ahead of print]. |