Surgical Insights for ODsIn the December 2024 issue of Review of Optometry—the magazine's 31st annual surgery report—learn how to spot and manage cataract surgery complications, review the newest techniques and procedures in refractive surgery and discover how laser procedures like SLT, LPI and YAG capsulotomy help your patients in the long term. Check out the other articles featured in this issue: |
With the current state of healthcare, optometrists are heavily involved in the comanagement of patients undergoing cataract surgery. Whether working with ophthalmologists in surgical practices or managing patients postoperatively in their own clinics, optometrists often share the burden of successful outcomes and patient satisfaction. It is of great importance, thus, for us to be well-versed in the complexities of post-surgical care and to be acutely aware of not only the common postoperative complications but also of how certain intraoperative issues may affect postoperative care and outcomes.
Intraoperative Complications
When seeing patients for their post-op appointments after cataract surgery, it is important to understand that not every surgery goes the same way. While most if not all patients get an intraocular lens (IOL) in place of their cloudy natural lens, the path to that IOL placement can often be vastly different. Without paying close attention to the surgical note, it is difficult to be fully aware of the hardships the surgeon faced during the procedure. Often, the result is excellent despite a challenging surgery. Though sometimes, signs of intraoperative complications may be present.
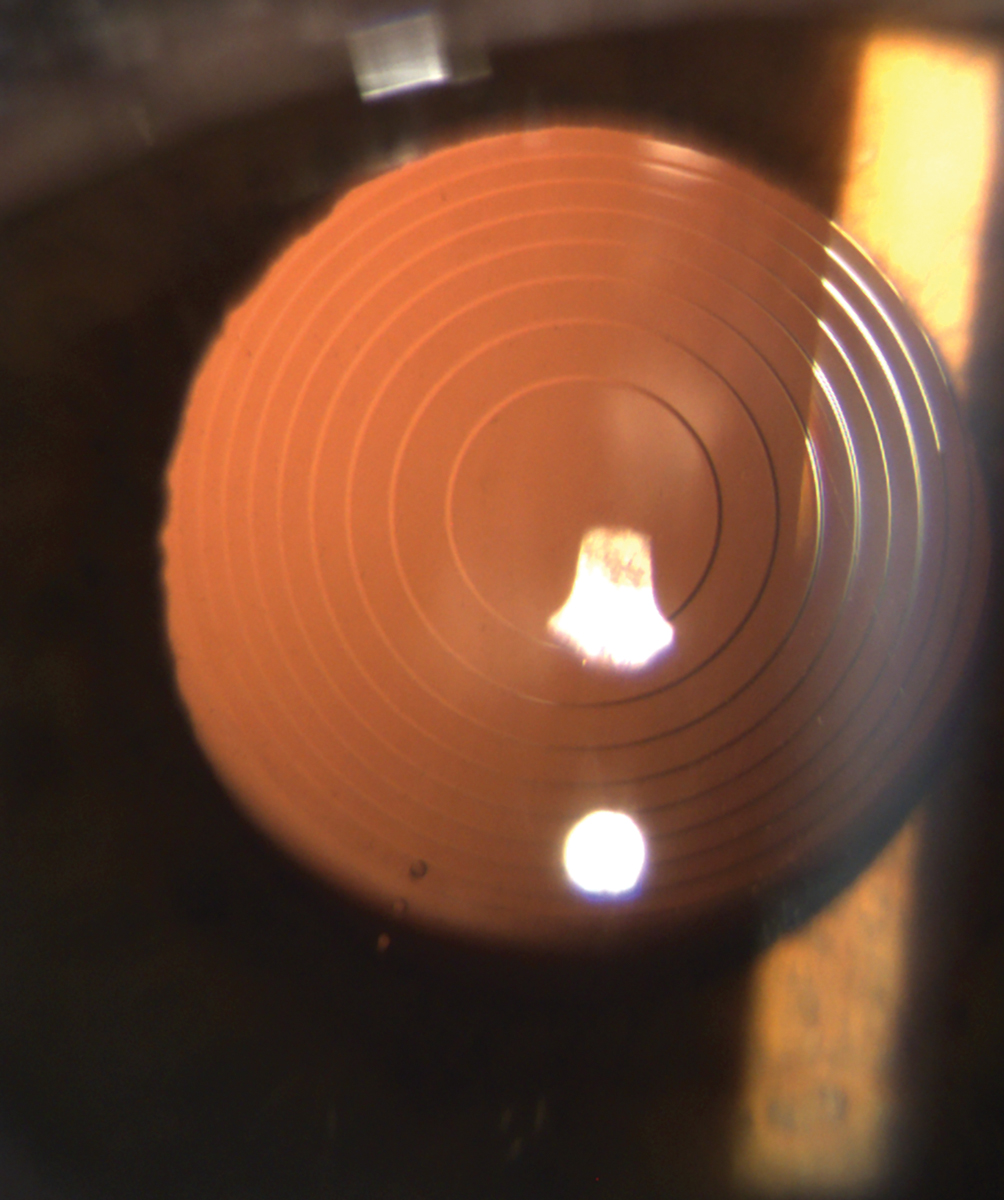
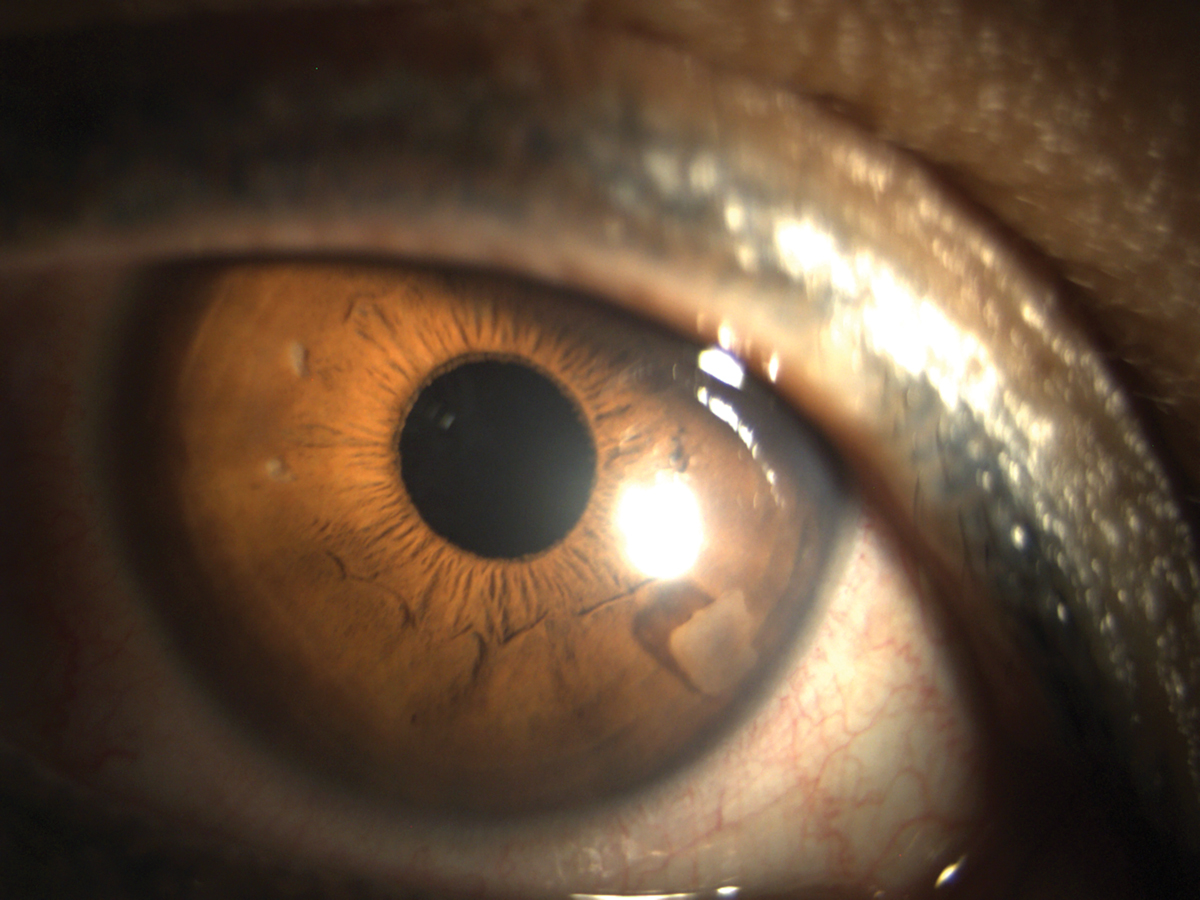
Posterior capsular rupture is a dreaded but relatively common intraoperative issue, with an occurrence rate of 0.45% to 5.2%.1,2 While it is impossible to always anticipate capsular rupture, recognizing the risk factors and careful planning reduces the possibility of it occurring. Those factors include the presence of posterior polar cataracts, pseudoexfoliation or very dense cataracts.2 Previous retinal surgeries or intravitreal injections may also increase the risk.3 A lens may be nicked accidentally during a retinal procedure, resulting in minor damage to the posterior capsule, which may not manifest into a problem until the stress of manual manipulation during the cataract surgery. Poor patient cooperation can also result in a capsular rupture, as eye movement during procedure creates an unstable surgical environment.
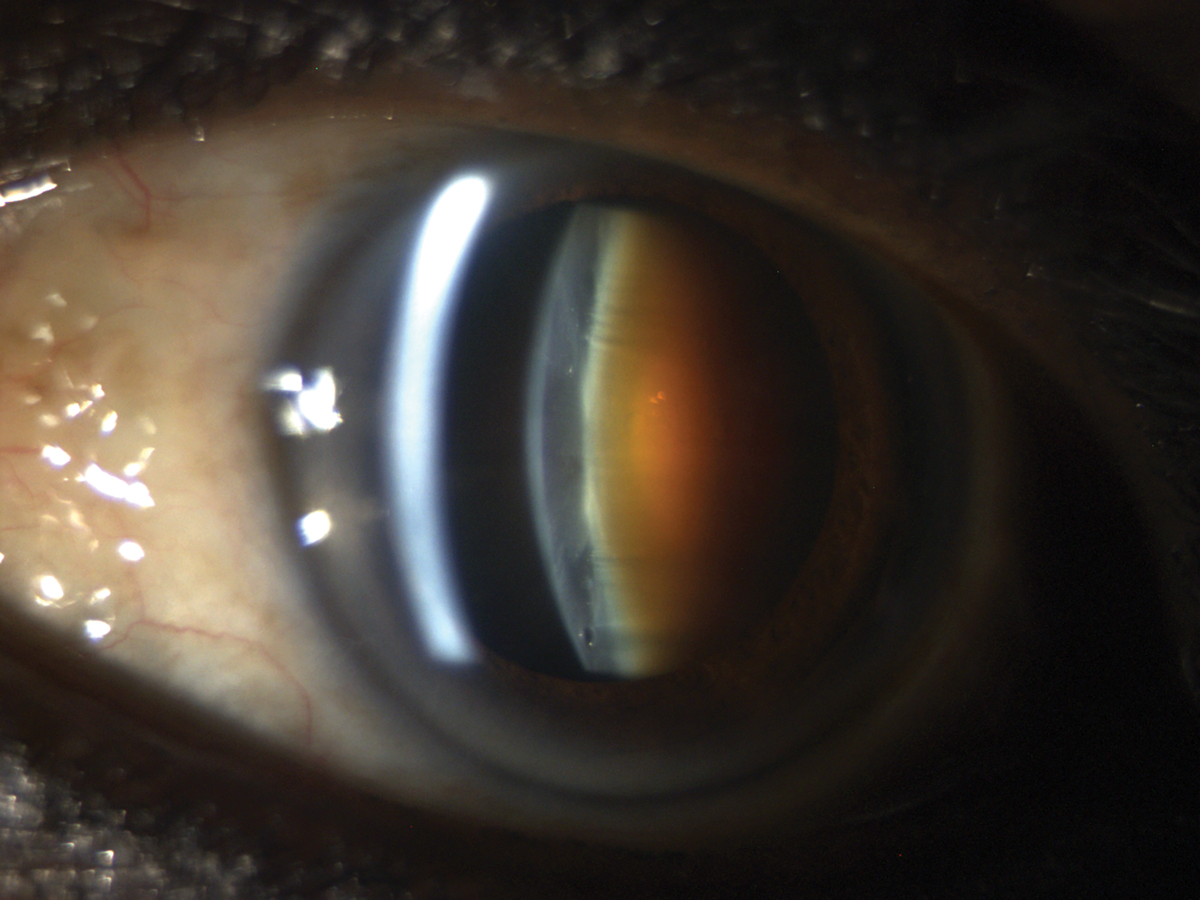
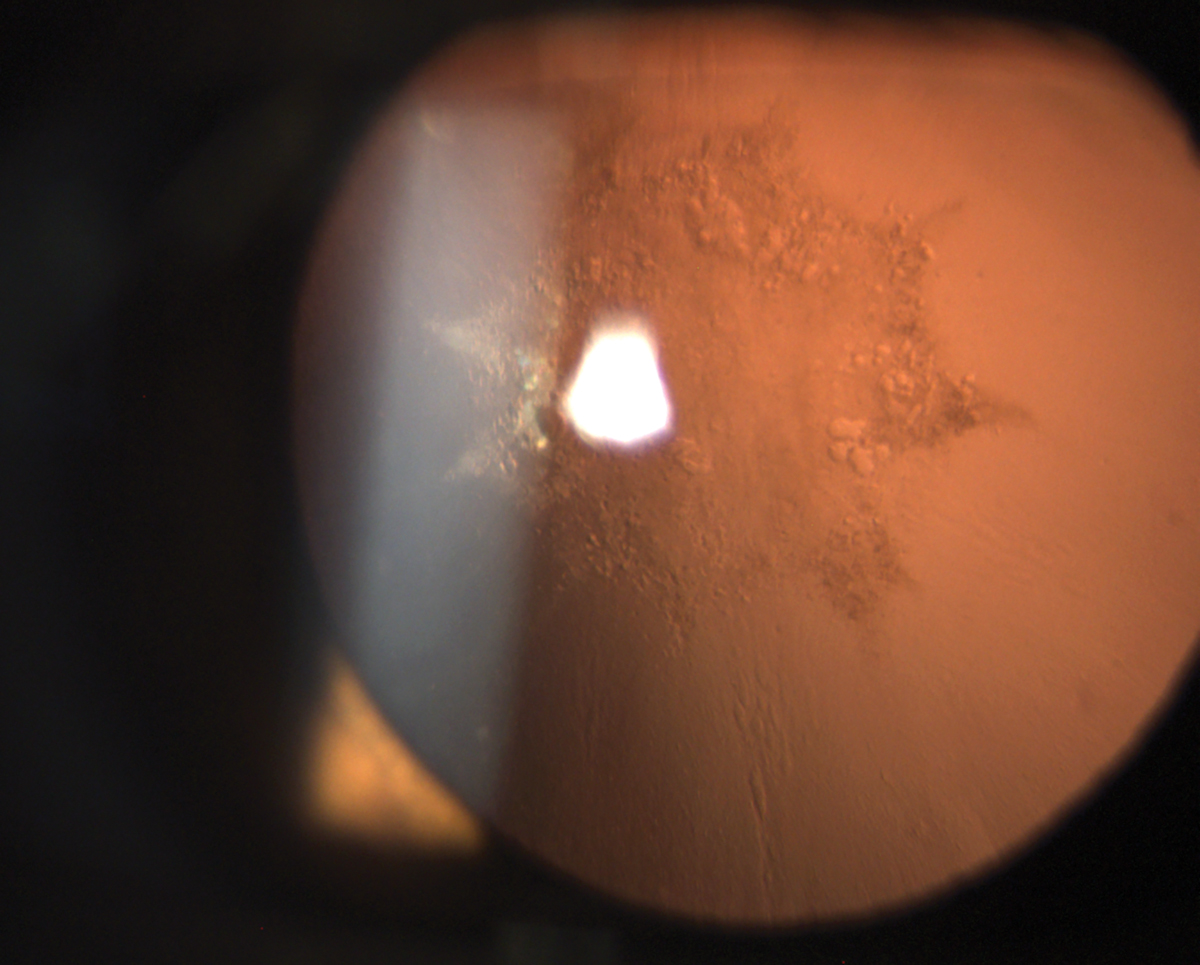
There are three main difficulties that may present with posterior capsular rupture: difficulty with IOL fixation, anterior vitreous prolapse and loss of lens material into vitreous.4 If vitreous comes forward anteriorly during the surgery, anterior vitrectomy is performed. Postoperatively, it is common to see white residue of intracameral steroid used to better visualize vitreous during the vitrectomy.5 If there is any concern for lenticular material in the vitreous, retinal specialist should be involved as soon as possible to determine if additional surgery is needed. The longer the lens material remains in the vitreous, the higher the risk of posterior complications, such as cystoid macular edema.6 If the IOL was placed properly, patients can still do well after vitrectomy and lens fragment removal.
If capsular integrity is compromised, placement of the IOL into the bag may not be possible. The IOL can still be fixated using primary or reverse optic capture (IOL optic being secured on one side of the capsule and haptics on the opposite side), or by placing a three-piece IOL in the sulcus. If there is not enough remaining capsular support for these options, scleral fixation may be considered. Unfortunately, with posterior capsular compromise, placement of premium IOLs may not be possible. This can be very frustrating to patients who were planning on receiving either a toric or a presbyopia-correcting IOL, only to be told after the surgery that they received a spherical single-focus IOL due to an intraoperative complication. As always, it is better to discuss a possibility of such scenario prior to surgery to avoid greater patient dissatisfaction.
 |
|
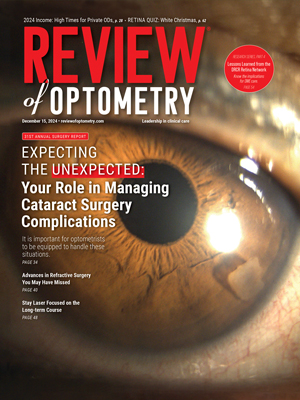
Cystoid macular edema should always be ruled out if best-corrected vision postoperatively does not meet preoperative potential. Click image to enlarge. |
It is not uncommon to see various iris defects postoperatively. They may present at transillumination defects, iris atrophy and/or pigmentary dispersion. These can arise from iris prolapse that needed to be swept back in during the surgery or from use of mechanical iris dilation tools in cases when pharmacological pupil dilation was not adequate. History of alpha-1 blockers increases the risk of floppy iris syndrome.7 Any patient known to take such medication would benefit from gentle hydrodissection and a more expert surgeon.
A rare, but visually threatening, surgical complication is suprachoroidal hemorrhage. It is thought to result from reduced intraocular pressure (IOP) during surgery, resulting in choroidal effusion with subsequent choroidal or ciliary vessel rupture.8 Though not always, suprachoroidal hemorrhage usually has an acute onset during the surgery. Anterior chamber shallowing, increased IOP, loss of red-light reflex and pain are common signs and symptoms of suprachoroidal hemorrhage.
Management of this condition involves immediate re-pressurization of the eye to increase IOP, even if the surgery is not complete.9 Depending on the severity of the hemorrhage, the surgeon will determine further course of action.
Postoperative Complications
Let’s review the potential situations that could occur in your post-cataract patients.
Wound leaks. These present early in the postoperative period and are incredibly concerning.
Signs of a wound leak include shallow anterior chamber, low IOP and a positive Seidel sign.10
Slow wound leaks in eyes with relatively deep anterior chambers can be observed closely. Wound scarring usually seals the leak over a course of a few days. Scarring can be facilitated by stopping the use of anti-inflammatory medication (steroids), switching the patient to an antibiotic that is less friendly to the ocular surface and placing a bandage contact lens over the eye.11 Aqueous suppressant eye drops may be used in conjunction.
 |
|
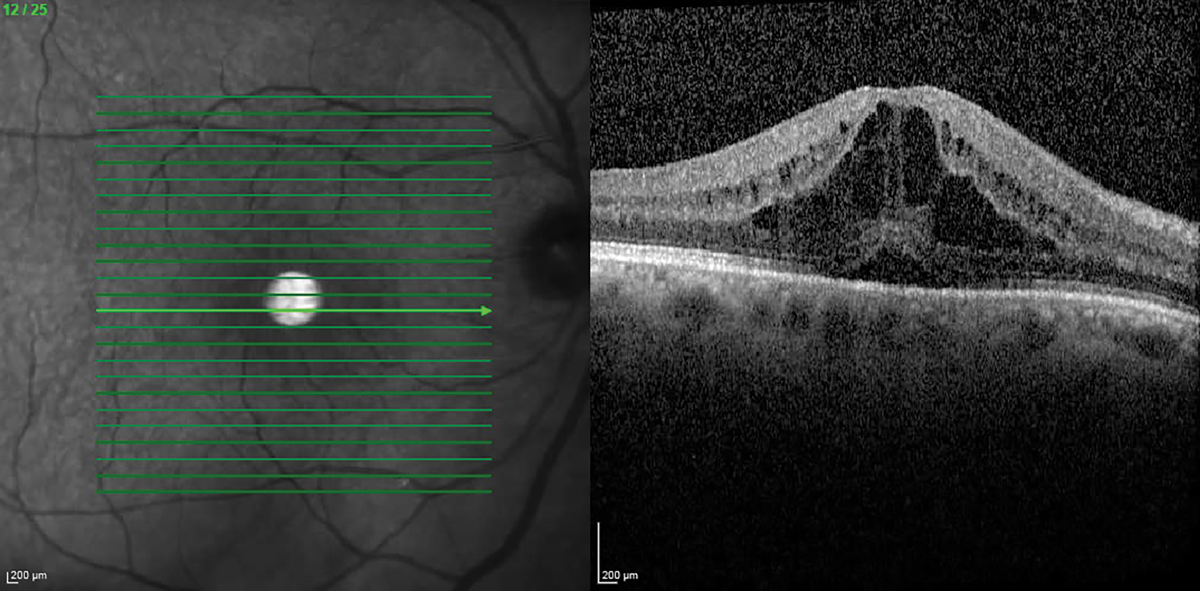
Diffractive extended depth-of-focus IOLs are more likely to cause dysphotopsias than single focus IOLs. Click image to enlarge. |
If the intraocular pressure is very low, anterior chamber is shallow and/or the leak is more severe in scale, surgical intervention may be needed. Each surgeon may have their own process, but some common interventions range from “hydrating the wound” (creating artificial corneal edema around the incision to allow for better seal) or placing one or more sutures to hold the wound closed until the scarring occurs (some sutures would need to be removed a few weeks later).12 Note that a tight suture may temporarily induce significant astigmatism, which resolves once the suture is removed.
Endophthalmitis. Inflammation of the aqueous and vitreous fluids due to an infection with bacteria or fungus after cataract surgery is a rare but severely sight-threatening complication.13 Symptoms of endophthalmitis include pain, redness and gradual loss of vision. Signs include prolific white blood cell reaction in aqueous and vitreous, as well as severe conjunctival hyperemia.14 Acute endophthalmitis presents within a few days to a few weeks after cataract surgery. Delayed-onset endophthalmitis can present over six weeks after surgery. Antimicrobial treatment needs to be started promptly. Cultures can aid diagnosis and choice of drug.
Residual refractive error. Technological advancements in the field of cataract surgery and the ability to achieve more and more precise refractive outcomes have brought with them the sky-high expectations from both patients and optometrists. It is important to understand that refractive surprises still occur about 12% to 15% of the time and are much more likely in patients with long or short axial lengths, previous corneal refractive surgery, irregular astigmatism (e.g., from keratoconus, corneal scarring or anterior basement membrane dystrophy), mature cataracts or poorly managed ocular surface disease and long-term previous contact lens wear (especially rigid gas-permeable lenses).15
Much should be done to optimize these contributing factors prior to surgery, but a perfect refractive outcome is never guaranteed. Despite knowing and understanding this truth, patients may be disappointed with their vision if their refractive target is not met. Thankfully, there are options to improve their visual outcome. IOL exchange and corneal refractive surgery such as LASIK or PRK can be performed in cases of significant residual refractive error. Procedure choice may depend on the amount of refractive surprise, corneal thickness, ocular surface health, type of IOL used and time elapsed since initial surgery, among other factors. A consultation with the surgeon is in order, though sometimes it may be prudent to wait a few weeks for refractive error to stabilize. Waiting too long is not ideal, as IOL exchange becomes significantly more difficult after three to six months due to capsular fibrosis.16
 |
|
Patients with dense cataracts are at higher risk of posterior capsular rupture. Click image to enlarge. |
An unexpectedly significant amount of astigmatism after surgery could be a result of toric IOL rotation. Checking the toric IOL axis to make sure it matches the planned axis is recommended within one to two weeks after cataract surgery. If toric IOL rotation is suspected, the patient can be sent back to the surgeon for the IOL to be rotated to the intended axis. Rarely, unexpected postoperative increase in astigmatism can be surgically induced by the creation of a corneal incision and resolve on its own over the course of a few weeks.
IOL decentration. This can be a result of zonular weakness from previous trauma or pseudoexfoliation, or IOL implantation issues, such as capsular rupture or failure of haptic to be positioned properly in-the-bag.17 A surgeon may choose to insert a capsular tension ring to compensate for the uneven force distribution among the zonules or address whatever other issue is causing the decentration.
Corneal edema. Cataract surgery is the most common cause of this condition. Corneal edema is associated with endothelial cell loss during phacoemulsification. Excess phacoemulsification power damages endothelial cells. Prolonged surgery may cause more stress to the cornea. Narrow anterior chamber and denser cataracts would increase the risk of corneal edema.
Viscoelastic substances may be used during the surgery to protect the endothelium, especially in eyes with preexisting endothelial damage or high risk of it during the surgery. Endothelial damage results in stromal edema, where most of the swelling occurs in the posterior cornea, often with resulting haze and endothelial folds. Another type of corneal edema, called microcystic edema, involves more anterior cornea. Microcystic edema is usually a result of elevated IOP. It is possible to see both types of edema in the same eye. Generally, corneal edema resolves over a few days. Rarely is it present a week after surgery. If stromal edema persists long-term (weeks or months), significant endothelial decompensation likely occurred. A consult with a corneal specialist should be considered.
 |
|
Small nuclear fragment in anterior chamber. Click image to enlarge. |
Elevated IOP.18 Causes of elevated postoperative IOP range from retained viscoelastic to steroid response to inflammation. It is important to identify the likely cause and select appropriate treatment. While retained viscoelastic is the most common cause of increased IOP at post-op day one, IOP that rises three to four weeks after surgery is likely due to steroid response.19
In most cases, a temporary addition of IOP-lowering medication is all that is needed to keep IOP under control. With inflammatory causes, increased anti-inflammatory treatment may be helpful. In cases where steroid response is suspected, reducing steroid administration frequency or switching to a milder steroid would be advised.
Cystoid macular edema (CME). The rate of this occurring following cataract surgery is under 2%.20,21 Patients with diabetes or macular pathology (e.g., epiretinal retinal membrane, previous macular edema) are more prone to CME development. Patients who develop CME are also more likely to be male, younger than age 65, Black, smokers and those with a history of uveitis.22
Treatment of CME may require a stepwise approach. First, steroid and NSAID drops (such as ketorolac or diclofenac) can be used. In a majority of cases without other comorbidities, this treatment is successful. Improvement and resolution of CME may take six to eight weeks. After the macula appears dry on OCT, medications can be tapered. Sub-tenon’s Kenalog (triamcinolone, Bristol-Myers Squibb) or intravitreal steroid (Ozurdex; dexamethasone intravitreal implant, Allergan) can be considered if topical medications do not elicit a response.23,24
Retinal detachment. One of the more vision-threatening complications of cataract surgery is retinal detachment, occurring after around 0.5% of surgeries.25 Younger age, male sex and longer axial length are significant risk factors. The increased risk of retinal detachment persists for up to 10 years after cataract surgery.26 Discussing this risk with patients is important, as is providing thorough education on symptoms of retinal detachment so that patients can seek care promptly.
Posterior capsular opacification (PCO). The diagnosis and management of PCO is rather straightforward. Nd:YAG laser capsulotomy can be performed, resulting in improvement with very little risk for the patient.27,28 If there is any chance of IOL exchange being needed in the future, the posterior capsule should be preserved.
IOL exchange is significantly more difficult after YAG capsulotomy and IOL options may also be limited due to increased difficulty of securing a new lens in the eye without the support of the posterior capsule. This is especially important if patients have a refractive surprise or they are not fully satisfied with their presbyopia-correcting IOL. In those cases, consultation with the surgeon should take priority over the YAG procedure.
 |
|
Posterior subcapsular cataracts increase the risk of PCO. Click image to enlarge. |
Dysphotopsias. Presence of these can be extremely bothersome to patients despite excellent visual outcome.29 Dysphotopsias occur because of light reflecting off the IOL onto the retina in a way that results in patients seeing unwanted visual phenomena. Dysphotopsias can be positive or negative in presentation.
Positive dysphotopsias are often described as light arcs, flashes, starbursts, halos or a shimmer. The hypothesized mechanism of positive dysphotopsias is stray light reflected off the IOL and concentrated on a specific area of the retina.30 Two factors associated with a higher risk of positive dysphotopsias are higher index of refraction of acrylic IOLs (the most commonly used IOL material currently), and the square IOL edge design of many modern IOLs (meant to reduce the rate of PCO formation).31,32 Most post-surgical dysphotopsias improve on their own over several weeks due to the process of neuroadaptation. The only management for most of these patients involves education and encouragement. For more symptomatic cases, pharmacologic miotic therapy such as brimonidine 0.15% or pilocarpine 0.5% may help.
If positive dysphotopsias do not improve with time (three to six months) or miotic therapy, surgical consult should be considered. Surgical treatment typically involves exchanging an IOL for one with a lower index of refraction (silicone or polymethyl methacrylate material), rounder edges, or a larger effective optic.33
Negative dysphotopsias are typically described as a dark peripheral “arc” or “crescent.” Some patients report a line or linear shadow, while others report a “strand of hair.” It is mostly noticed in the temporal field of vision. Light interacting with the sharp edge of the IOL at a specific angle results in a shadow on the nasal retina, affecting temporal visual field.34 The vast majority of symptomatic patients note significant improvement in symptoms or a complete resolution within three to six months. If negative dysphotopsias continue to be bothersome and show no signs of improvement, surgical intervention may be considered.
Reverse optic capture of current IOL (optic of the IOL is lifted above the capsulorhexis, while the haptics remain in the bag) or placement of a three-piece IOL in the sulcus are the most effective treatments options.35 Both of these procedures result in a more anterior IOL position, thus changing the angle at which the light interacts with the IOL edge. It is important to warn the patient that changing the position of the IOL more anteriorly will also slightly change the refractive outcome.
Presbyopia-correcting IOLs. Patients who receive these IOLs may have higher expectations and lower tolerance for imperfections given the high additional cost and the “premium” product label. The most common cause of dissatisfaction in patients with multifocal implants is residual refractive error, followed by dry eye, glare and halos.36 Quality of vision and severity of dysphotopsias is usually more favorable with extended depth-of-focus IOLs, but uncorrected near vision is better with multifocal IOLs. Myopic residual refractive error can be enhanced with corneal refractive surgery. Significantly hyperopic outcomes may benefit more from an IOL exchange.
Despite an otherwise perfect result, some patients just do not tolerate the optics of presbyopia-correcting IOLs, reporting blurry vision and/or significant dysphotopsias. In the absence of other significant issues, an exchange for a single-focus IOL should be considered. Waiting two to three months for neuroadaptation to occur is prudent, but waiting longer than six months will make an IOL exchange more difficult. Referral should be made back to the surgeon in that time frame.
Takeaways
Even though cataract surgery has been around for quite a while, it continues to evolve. While surgical complications are not desired, they happen. It is important for ODs to maintain clinical expertise, continue providing excellent perioperative care and work together with ophthalmologists to achieve great patient outcomes and satisfaction.
Dr. Sukhovolskiy is a staff optometrist at Pacific Cataract and Laser Institute, practicing in Tacoma, WA. He has no financial disclosures.
1. Greenberg PB, Tseng VL, Wu WC, et al. Prevalence and predictors of ocular complications associated with cataract surgery in United States veterans. Ophthalmology. 2011;118(3):507-14. 2. Sim PY, Donachie PHJ, Day AC, Buchan JC. The Royal College of Ophthalmologists' National Ophthalmology Database study of cataract surgery: Report 17, a risk factor model for posterior capsule rupture. Eye (Lond). September 19, 2024. [Epub ahead of print]. 3. Zhong Z, He Z, Yu X, Zhang Y. Intravitreal injection is associated with increased posterior capsule rupture risk during cataract surgery: a meta-analysis. Ophthalmic Res. 2022;65(2):152-61. 4. Ti SE, Yang YN, Lang SS, Chee SP. A 5-year audit of cataract surgery outcomes after posterior capsule rupture and risk factors affecting visual acuity. Am J Ophthalmol. 2014;157(1):180-185.e1. 5. Yamakiri K, Uchino E, Kimura K, Sakamoto T. Intracameral triamcinolone helps to visualize and remove the vitreous body in anterior chamber in cataract surgery. Am J Ophthalmol. 2004;138(4):650-2. 6. Lin WV, Scott MN, Tendhar C, et al. Outcomes of cataract surgery complicated by retained lens fragments requiring pars plana vitrectomy. Clin Ophthalmol. 2020;14:939-46. 7. Saad M, Maisch N. Alpha blocker-associated intraoperative floppy iris syndrome. Sr Care Pharm. 2022 ;37(6):227-31. 8. Flores Márquez A, Urbinati F, Rocha-de-Lossada C, et al. Management of suprachoroidal hemorrhage during phacoemulsification: a comprehensive review. Medicina (Kaunas). 2023;59(3):583. 9. Savastano A, Rizzo S, Savastano MC, et al. Choroidal effusion and suprachoroidal hemorrhage during phacoemulsification: intraoperative management to prevent expulsive hemorrhage. Eur J Ophthalmol. 2016;26(4):338-41. 10. Matossian C, Makari S, Potvin R. Cataract surgery and methods of wound closure: a review. Clin Ophthalmol. 2015;9:921-8. 11. Astbury N, Nyamai LA. Detecting and managing complications in cataract patients. Community Eye Health. 2016;29(94):27-9. 12. Tong AY, Gupta PK, Kim T. Wound closure and tissue adhesives in clear corneal incision cataract surgery. Curr Opin Ophthalmol. 2018;29(1):14-8. 13. Chen G, Tzekov R, Li W, et al. Incidence of endophthalmitis after vitrectomy: a systematic review and meta-analysis. Retina. 2019;39(5):844-52. 14. Wadbudhe AM, Tidke SC, Tidake PK. Endophthalmitis after cataract surgery: a postoperative complication. Cureus. 2022;14(10):e30110. 15. Brogan K, Diaper CJ, Rotchford AP. Cataract surgery refractive outcomes: representative standards in a National Health Service setting. Br J Ophthalmol. 2019;103(4):539-43. 16. Märker DA, Radeck V, Barth T, et al. Long-term outcome and complications of IOL-exchange. Clin Ophthalmol. 2023;17:3243-8. 17. Chen XY, Wang YC, Zhao TY, et al. Tilt and decentration with various intraocular lenses: a narrative review. World J Clin Cases. 2022;10(12):3639-46. 18. Grzybowski A, Kanclerz P. Early postoperative intraocular pressure elevation following cataract surgery. Curr Opin Ophthalmol. 2019;30(1):56-62. 19. Bojikian KD, Nobrega P, Roldan A, et al. Incidence of and risk factors for steroid response after cataract surgery in patients with and without glaucoma. J Glaucoma. 2021;30(4):e159-63. 20. Chu CJ, Johnston RL, Buscombe C, et al. Risk factors and incidence of macular edema after cataract surgery. Ophthalmology. 2016;123(2):316-23. 21. Iftikhar M, Dun C, Schein OD, et al. Cystoid macular edema after cataract surgery in the United States. IRIS Registry (Intelligent Research in Sight) analysis. Ophthalmology. 2023;130(10):1005-14. 22. Chu CJ, Johnston RL, Buscombe C, et al.; United Kingdom Pseudophakic Macular Edema Study Group. Risk factors and incidence of macular edema after cataract surgery: a database study of 81,984 eyes. Ophthalmology. 2016;123(2):316-23. 23. Lavaud A, Nicolau R, Brezin AP. Subtenon injection of triamcinolone acetonide as first-line treatment of postoperative clinically significant pseudophakic cystoid macular edema. Invest Ophthalmol Vis Sci 2015;56:173. 24. Tabg B, Shen Yeow CE, Harney F, Townley D. Safety and effectiveness of intravitreal dexamethasone implant (Ozurdex) for the treatment of refractory cystoid macular oedema (CMOP) in Galway University hospital. Open Ophthalmol J. 2022;16:e187436412210210. 25. Thylefors J, Jakobsson G, Zetterberg M, Sheikh R. Retinal detachment after cataract surgery: a population-based study. Acta Ophthalmol. 2022;100(8):e1595-9. 26. Qureshi MH, Steel DHW. Retinal detachment following cataract phacoemulsification-a review of the literature. Eye (Lond). 2020;34(4):616-31. 27. Grzybowski A, Kanclerz P. Does Nd:YAG capsulotomy increase the risk of retinal detachment? Asia Pac J Ophthalmol (Phila). 2018;7(5):339-44. 28. Joshi RS, Doble P. The complication rate following neodymium-doped yttrium aluminum garnet laser posterior capsulotomy for posterior capsular opacification in patients with and without comorbidities. Indian J Ophthalmol. 2023;71(3):791-6. 29. Kinard K, Jarstad A, Olson R. Correlation of visual quality with satisfaction and function in a normal cohort of pseudophakic patients. J Cataract Refract Surg. 2013;39(4):590-7. 30. Erie JC, Bandhauer MH, McLaren JW. Analysis of postoperative glare and intraocular lens design. J Cataract Refract Surg. 2001;27(4):614-21. 31. Davison JA. Positive and negative dysphotopsia in patients with acrylic intraocular lenses. J Cataract Refract Surg. 2000;26(9):1346-55. 32. Holladay JT, Lang A, Portney V. Analysis of edge glare phenomena in intraocular lens edge designs. J Cataract Refract Surg. 1999;25(6):748-52. 33. Masket S, Rupnick Z, Fram NR, et al. Surgical management of positive dysphotopsia: US perspective. J Cataract Refract Surg. 2020; 46(11):1474-9. 34. Holladay JT, Zhao H, Reisin CR. Negative dysphotopsia: the enigmatic penumbra. J Cataract Refract Surg. 2012;38(7):1251-65. 35. Masket S, Fram NR, Cho A, et al. Surgical management of negative dysphotopsia. J Cataract Refract Surg. 2018; 44(1):6-16. 36. Gibbons A, Ali TK, Waren DP, Donaldson KE. Causes and correction of dissatisfaction after implantation of presbyopia-correcting intraocular lenses. Clin Ophthalmol. 2016;10:1965-70. |