 |
|
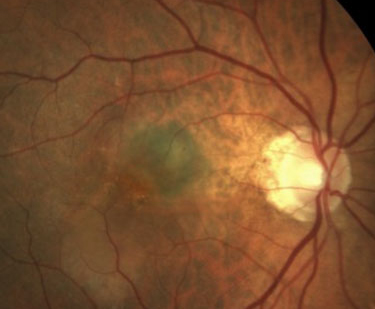
A recent study published in Eye investigates the demographic representation in clinical trials for AMD. While female subject enrollment was found to align with the burden of disease, the study revealed a notable underrepresentation of racial and ethnic minorities, including Black, Hispanic, and Asian participants. The findings stress the importance of ensuring diverse enrollment in future AMD trials to enhance the generalizability of treatment outcomes and address health equity in ophthalmic research. Photo: Jessica Haynes, OD. Click image to enlarge. |
Most decisions made by eyecare providers are informed by clinical trial outcomes, trusting that the safety and efficacy of a given product can be extended to all relevant patient populations. However, recent studies have revealed enrollment disparities, suggesting decreased confidence in the demographic representation of real-world populations. When considering ophthalmic diseases such as age-related macular degeneration (AMD), which disproportionately affects women, researchers wondered if enrollment was equitable. Their findings were recently published in the journal Eye, showing female enrollment in clinical trials for AMD to be commensurate with their disease burden, but a severe under-reporting of enrollment for minority racial and ethnic groups exists.
The cross-sectional study included 106 trials from clinicaltrials.gov spanning 1990 to 2020, totaling 77,939 patients, of which 46.3% were female. Researchers calculated pooled population-to-prevalence ratios (PPRs) from the Global Burden of Disease database and determined an equitable PPR trial enrollment between 0.8 and 1.2. Secondary outcomes included absolute number of enrolled female, racial and ethnic groups, and the association of trial characteristics with these demographics.
Ultimately, the pooled female PPR was 0.88, and most trial characteristics fell within the equitable values. While the absolute enrollment of female subjects (46.3%) was within the acceptable range, researchers said they were still the lesser included biological sex, albeit by a small margin. Other studies have shown conflicting sex-based enrollment, including higher rates of male subject enrollment for diseases such as diabetic macular edema, as well as an over- or equally represented rate of female patients in clinical trials for presbyopia and cataracts, respectively. “Given this literature, our results further corroborate the variability of female enrollment into trials based on the ocular disease and also indicate equitable generalizability of AMD trial results for female sex in the study period,” wrote the authors in their paper. “While further investigation is needed on the role of biological sex on the clinical course of AMD, sex-based enrollment parity in AMD trials should continue to be prioritized as newer treatments are developed.”
Researchers determined 74 of the clinical trials adequately detailed subjects’ race/ethnicity. White participants comprised the largest group (82%), followed by Black or African American (7.4%), unreported (6%), Hispanic (4.3%) and Asian (4.2%). The authors said in their paper that several factors may contribute to this inequity, including a broad mistrust of the medical system and financial restraints due to historical inequities, as well as a concurrent overrepresentation of high-income groups enrolled in clinical trials, which has been reported by the World Health Organization.
The authors also mention the lack of geographic status in clinical trials. “For instance, rural geographic status is a barrier to care, and within the research context, evidence supports that clinical trial sites are frequently clustered in urban areas, especially within the coastal United States,” they wrote in Eye. “To promote equitable enrollment and potentially reveal geography-dependent differences in treatment response, study investigators may consider expanding trial sites to more rural and underserved communities.”
Although the researchers say it may consider use of trials solely from clinicaltrials.gov as a limitation, which inherently leaves out the broader corpus of AMD literature, they said this method was more likely to capture Western trials, which more often enroll patients from demographic-diverse regions.
In conclusion, while female subjects were enrolled in AMD clinical trials in acceptable proportions in the eyes of the researchers, the racial and ethnic minority group reporting was lower than ideal. “To improve the generalizability of high-quality evidence on AMD interventions, future trials should enroll participants in approximation to real-world disease burden across all demographics,” they wrote. “As well, further investigation is needed to identify trials of ophthalmic conditions with insufficient enrollment of patient demographics groups, in order to ensure that future efforts are directed towards appropriately reflecting demographic-related disease burden in study populations.”
| Click here for journal source. |
Tao, BK, Xie, JS, Leung, V et al. Enrolment characteristics in age-related macular degeneration clinical trials: A cross-sectional study. Eye. December 27, 2024. [Epub ahead of print.] |



