 |
|
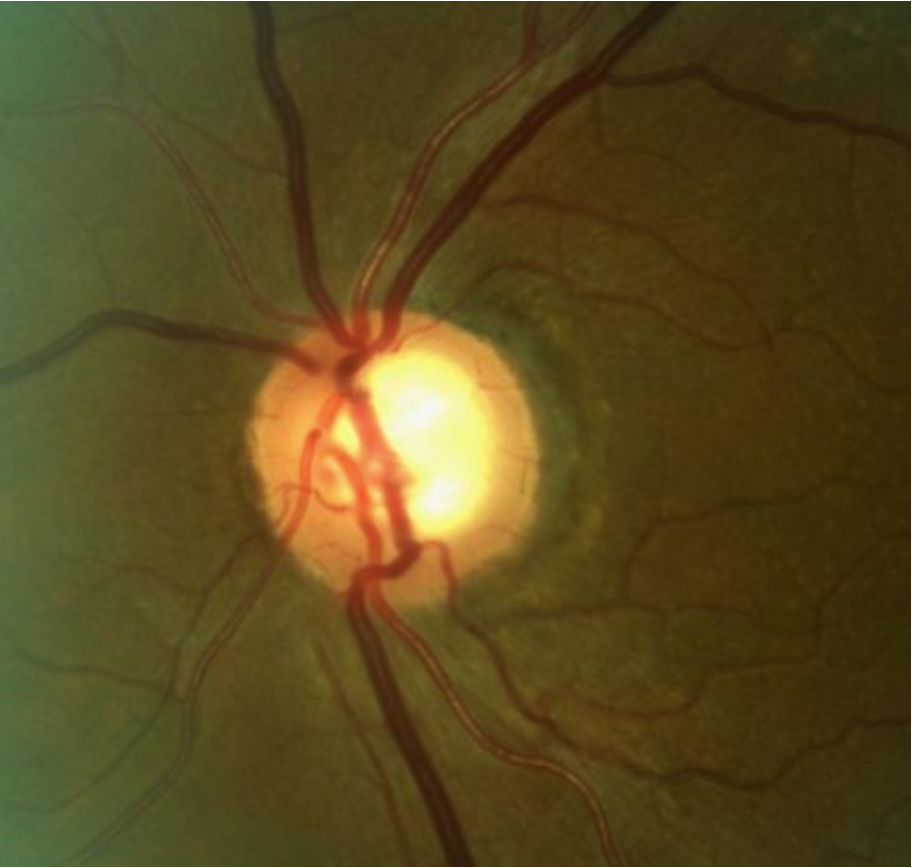
In this study, underdiagnosis of POAG was more common than overdiagnosis. Of the 13.8% of subjects who experienced a diagnostic change within two years after their initial visit—upstaging from POAG suspect to POAG or vice versa—77.9% involved cases of advancing disease. Photo: Andrew Rixon, OD. Click image to enlarge. |
Proper staging of glaucoma is crucial to inform treatment paradigms and follow-up frequency. Despite improvements in strategies and imaging for disease detection over the years, misdiagnosis remains fairly common, especially among primary open-angle glaucoma (POAG) and POAG suspects (POAGS). To provide clinicians with a structured approach for diagnosing and managing these patients, the American Academy of Ophthalmology set forth Preferred Practice Patterns in 2020. These guidelines delineate specific clinical findings and risk factors that suggest an increased possibility of developing POAG, which include either (1) elevated intraocular pressure without visible optic disc or retinal nerve fiber layer (RNFL) abnormalities, (2) optic nerve or RNFL that is suspicious for glaucomatous damage or (3) visual field defects that suggest damage but aren't explained by other pathologies.
Because the decision to treat a glaucoma patient or suspect is nuanced, and no studies have elucidated the accuracy of eyecare providers applying these definitions when staging patients, a group of researchers recently sought to fill this gap. They performed a retrospective, single-site, case-control study on patients aged 40 and older diagnosed with POAG or POAGS, who were followed for a minimum of 24 months. Subjects who did not experience a diagnostic change during this time were labeled as controls, while those who changed from glaucoma to suspect or vice versa in the two-year period were referred to as cases. Clinical data were analyzed to assess the main outcome measure, which was “to determine if baseline characteristics, type of provider seen or ophthalmic testing performed were protective or risk factors in regards to diagnostic change,” the authors wrote in their study for Ophthalmology Glaucoma.
A total of 922 subjects were included, with an incidence of diagnostic changes at 13.8%. Among these, 99 subjects were upstaged from POAGS to POAG, while 28 changed from POAG to POAGS. Put another way, more than three-quarters of diagnostic changes (77.9%) involved cases advancing from POAGS to POAG, “highlighting that underdiagnosis of disease was more common than overdiagnosis,” the researchers explained. Importantly, they also reported that “72% POAGS to POAG subjects were left untreated with either prescription antihypertensive medications or laser trabeculoplasty between the initial and follow-up visits.”
The occurrence of non-glaucomatous visual field defects was significantly higher in cases compared to controls. Through regression analysis, the study authors determined that this finding increased the odds of diagnosis changes. No other baseline factors increased risk, that list including age, sex, race, hypertension, diabetes, autoimmune disease, family history of glaucoma, spherical equivalent or prior cataract surgery.
Eyecare provider type also appeared to affect outcomes. Cases were significantly less likely to be seen by a glaucoma specialist during the initial visit compared to controls, and fewer cases underwent visual field testing, OCT testing or gonioscopy at that visit than controls. Multivariate analysis indicated that performing visual fields or OCT at both visits reduced the odds of short-term diagnostic change, while switching from a non-glaucoma specialist to a glaucoma specialist between visits increased the odds of diagnostic change.
“Due to the insidious nature of glaucoma progression, both underdiagnosis and overdiagnosis can be a significant challenge,” the researchers conveyed. “Our study highlights the importance of not solely relying on one diagnostic test and taking caution to avoid interpreting results in isolation.” Equally important, they noted, is having these results interpreted by experienced and well-trained providers.
Reflecting on all of these findings, the researchers stated, “The examinations recommended by the AAO during visits are essential for protecting against diagnostic changes,” noting that these include gonioscopy, pachymetry, tonometry, perimetry, optic nerve examination and optic nerve head imaging. “All of these tests are important in correctly diagnosing, staging and monitoring glaucoma states,” they wrote. “Therefore, adherence to performing these exams is critical to minimize short-term diagnostic changes.”
| Click here for journal source. |
To LK, Carrabba NV, Kalathuru CG, et al. Risk factors for diagnostic change from glaucoma suspect to primary open-angle glaucoma and vice versa over two years. Ophthalmol Glaucoma. December 20, 2024. [Epub ahead of print]. |



