 |
|
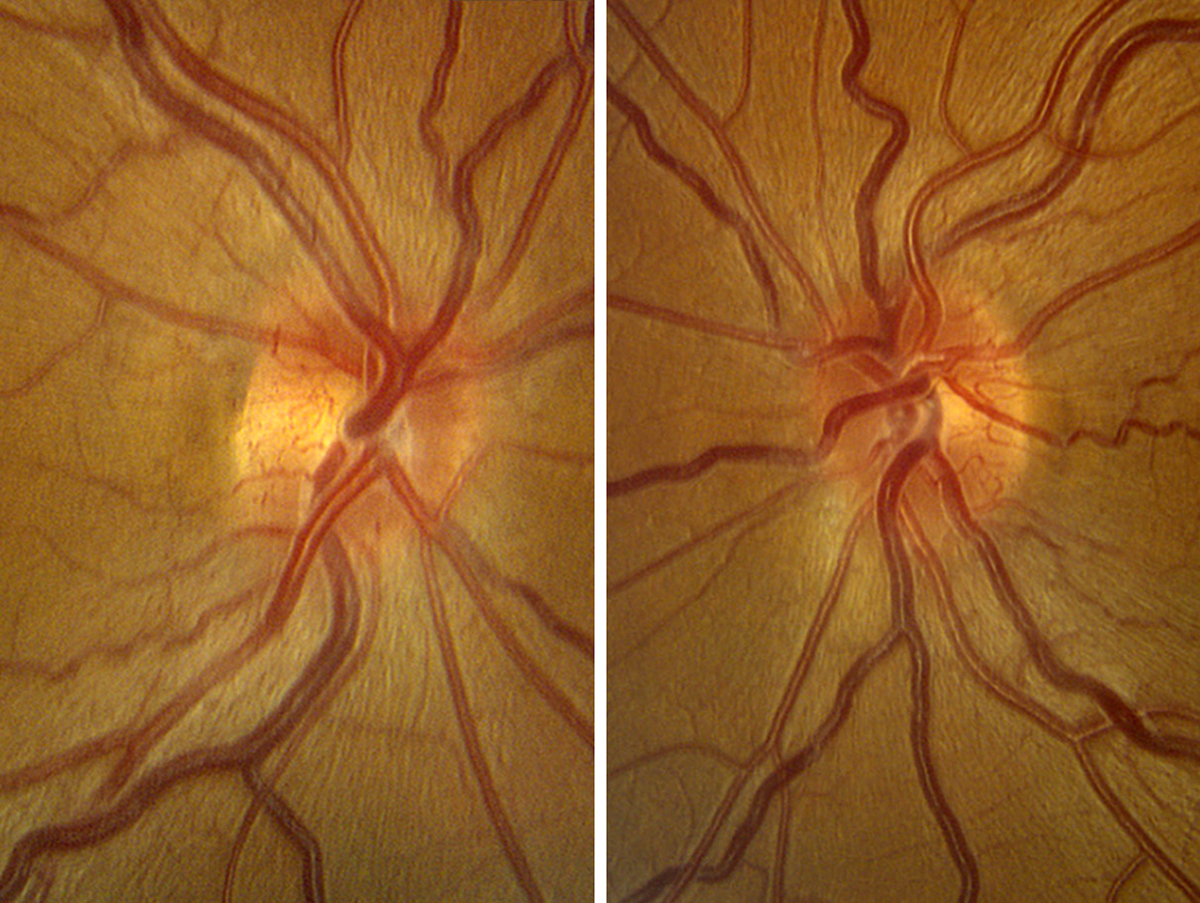
Long-term safety of gene therapy is a critical consideration, with potential risks of immune responses, off-target effects or unintended consequences of gene insertion. Over five years, 124 intraocular inflammation events occurred in the injected eyes, with 94% observed in the first two years. Photo: Alison Bozung, OD. Click image to enlarge. |
After the success of voretigene neparvovec for Leber’s congenital amaurosis, the somewhat related condition of Leber’s hereditary optic neuropathy (LHON) has more recently been studied as another possible gene therapy target. Patients may experience abrupt, painless vision loss, with severe impairment often developing quickly—prompting researchers to investigate new avenues for therapy. In one recent paper published by JAMA Ophthalmology, lenadogene nolparvovec was analyzed for safety and efficacy five years after injection for those with LHON due to the MT-ND4 gene variant.
The five-year follow-up study included two Phase III clinical studies—RESCUE and REVERSE—which analyzed lenadogene nolparvovec for efficacy up to six months and from seven months to one year after onset, respectively. At the end of each two studies (after two years), patients were offered to enroll in the RESTORE trial for another three years of follow-up. Of the 76 patients in the RESCUE and REVERSE studies, 81.6% decided to move forward with the RESTORE trial, and 72.4% of this cohort completed the five-year follow-up. Baseline best-corrected visual acuity (BCVA) was on average 1.5logMAR in eyes to be treated with the agent and 1.4 logMAR in sham eyes. Mean change from baseline to year two was -0.05 logMAR, or +1 line, in the therapy-treated eyes; however, after five years, bilateral improvement from the worst BCVA recorded was similar to the two-year observation, with mean change of -0.4 logMAR, or more than +4 lines of improvement, for eyes treated with the agent as well as the same average occurring for sham eyes. Improvement from worst BCVA of at least -0.3 logMAR, or +3 lines, was seen in 66.1% of patients. Between two to five years, intraocular inflammation occurred in four people with eight events in treated eyes and one event in the sham group.
The authors of the paper do note in their discussion that baseline BCVA can vary greatly depending on disease stage and time of patient enrollment, thus making this measure an unsuitable reference point for meaningful comparison between and within study. Consequently, they used nadir as a more stable reference value in assessing treatment effect.
As for the observation of improvement in sham eyes, nonclinical investigations have been conducted to elucidate potential mechanisms. In healthy monkeys, r lenadogene nolparvovec delivered via adeno-associated virus (AAV) was able to transfer from injected to uninjected eyes. As well, an mRNA transgene was expressed in the contralateral eye of mice after unilateral injection. Postmortem study of two RESCUE patients revealed 6.5 years after treatment that the AAV2-ND4 transgene was found in retinas of both injected and sham eyes.
Overall, the authors relay that “these results demonstrate the persistent benefit over time from a single dose of lenadogene nolparvovec, which is promising for the use of gene therapy in LHON due to the MT-ND4 gene variant.”
However, an invited commentary, also published by JAMA Ophthalmology, points to the durable effect possibly being due to the researchers choosing worst BCVA to look at rather than baseline BCVA. As the commentary authors explain, “such analyses almost certainly overestimate the amount of improvement because one poor VA measurement may represent a one-time event due to poor effort or poor fixation, not represent the true BCVA, so that subsequent BCVA improvements may not represent true improvements, and may also account for why improvements were seen in both eyes.”2
Instead, they suggest that investigators who insist on using worst-case status when assessing treatment effect should require two consecutive visits that confirm stability, as well as consider changes from baseline. They also add that when investigating diseases where BCVA at enrollment may be low, like with LHON, that definitive BCVA changes may be considered to be at least six lines, in contrast with at least two or three lines of BCVA for conditions like diabetic macular edema, in which average baseline logMAR is much better.
Despite these criticisms, the commentators do believe that, “nevertheless, AAV vector trafficking to the noninjected eye may be unique to retinal ganglion cell gene therapy, as it has not been observed in photoreceptor- or retinal pigment epithelium-directed gene therapies.”2
| Click here for journal source. |
1. Yu-Wai-Man P, Newman NJ, Biousse V, et al. Five-year outcomes of lenadogene nolparvovec gene therapy in Leber hereditary optic neuropathy. JAMA Ophthalmol. December 19, 2024. [Epbu ahead of print]. 2. Scholl HPN, György B. Single-eye gene therapy for Leber hereditary optic neuropathy. JAMA Ophthalmol. December 19, 2024. [Epub ahead of print]. |



