 |
|
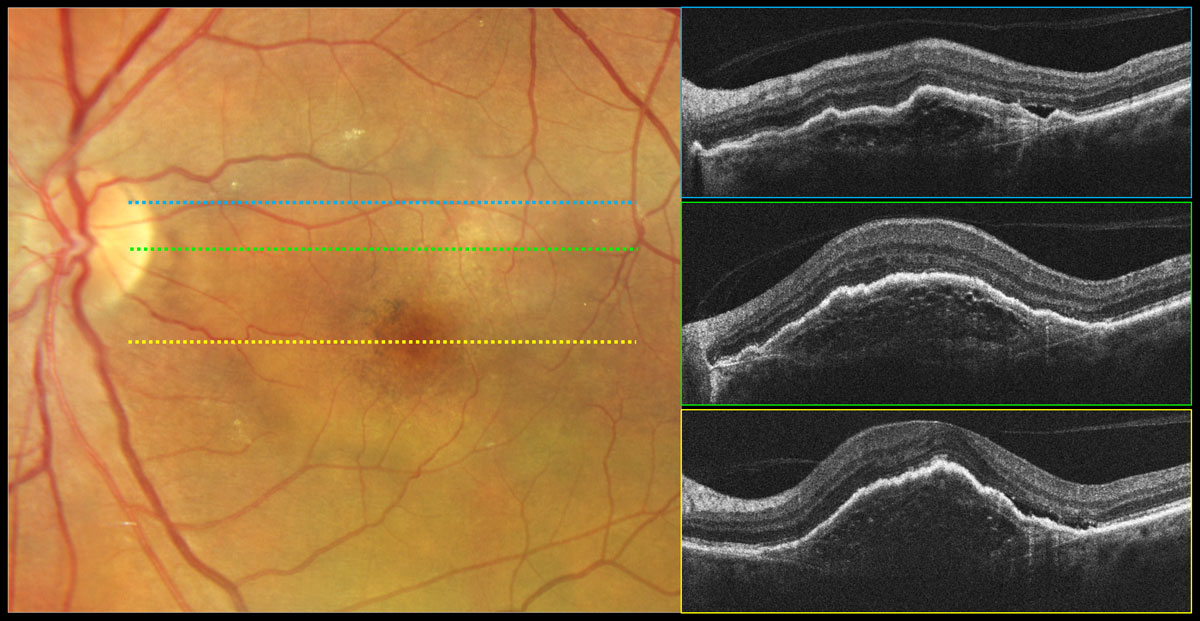
This global survey of more than 6,000 people in 24 countries provides new and important insights into the breadth and depth of the challenges and opportunities in the optimal delivery of care and management of patients with wet AMD. Addressing these challenges in the healthcare community can all serve to improve vision outcomes for patients and ultimately quality of life. Photo: Carolyn Majcher, OD. Click image to enlarge. |
Today’s treatments can help many patients with neovascular age-related macular degeneration (wet AMD) maintain reasonably good central vision. Understanding and addressing barriers to anti-VEGF treatment is an important goal in optimizing these outcomes. To address these questions and gaps, and to further understand the challenges and develop potential solutions, the Barometer Program, an international coalition of experts in retinal disease, vision care and aging, conducted a global survey amongst patients with wet AMD, healthcare providers and associated clinic staff. This global survey highlighted the breadth of obstacles associated with clinical management of patients with this condition. Challenges included disease and appointment burden, understanding of disease/anti-VEGF treatment and setting expectations. Opportunities included improving quality and access to educational materials for patients, enabling better doctor-patient conversations and supporting patients in attending their appointments. These findings were published in Ophthalmology and Therapy.
A survey was carried out of patients with neovascular age-related macular degeneration, their providers and clinic staff in 77 clinics across 24 countries on six continents, from a diverse range of healthcare systems, settings and reimbursement models. Data gathered included patient personal characteristics, appointment attendance challenges, treatment experiences and opportunities to improve support. Provider and clinic staff surveys asked similar questions about their perspectives. There were 6,425 responses: 4,558 patients with wet AMD, 659 providers and 1,208 clinic staff.
The study identified that potential barriers included the high frequency of treatment (45.9% of patients) concern about being a burden to family/friends (44%), personal costs related to the therapy (42.3%),difficulties in traveling to appointments (39.6%), long waiting times (39.9%) and insufficient comprehension of the condition (24.8%). Participants identified logistical (improved financial assistance with treatment and out-of-pocket costs, as well as appointment reminders), operational (addressing clinic setup to reduce waiting times and improving the amount of time providers spend with patients) and educational (improving quality and provision of patient information and expectation-setting) opportunities to improve care.
The study authors noted that patients who do not understand the goals of their treatment could likely become dissatisfied (many patients expect their vision to significantly improve with treatment, whereas maintenance of vision might be a more suitable goal) and become nonadherent. “Expectations must be carefully set early in the patient’s treatment journey,” they suggested in their paper. “Leveraging waiting times for appropriate staff to provide additional education or improving communications training for providers and clinic staff may be ways to aid in educating patients and improving their expectations.”
| A similar survey on DME treatment burdens was published in the same issue. Our summary of it can be found here. |
Still, no consensus appears to exist for how and when to appropriately communicate specific information at different stages of the patient’s treatment journey. The study authors recommended materials to guide patients and providers on when to ask or answer questions specific to different stages in the patient’s disease and treatment that could help alleviate any miscommunication and ensure that patients are better informed about what they can expect with treatment.
“These data can also help to improve clinic efficiency and capacity, allowing healthcare providers to have additional time for discussion to ensure that patients understand the need, frequency and expectations of treatment,” the team concluded.
| Click here for journal source. |
Loewenstein A, Sylvanowicz M, Amoaku WM, et al. Global insights from patients, providers, and staff on challenges and solutions in managing neovascular age‑related macular degeneration. Ophthalmol Ther. December 14, 2024. [Epub ahead of print]. |



