The heightened risk of developing open-angle glaucoma (OAG) in myopic eyes may stem from the mechanical stress caused by eye elongation, which also contributes to optic nerve head deformation and presents as disc tilt, rotation and β-zone parapapillary atrophy. A new study recently explored the impact of optic disc rotation—specifically, its relationship to visual field (VF) defects in myopic eyes with OAG. Its findings, recently published in Graefe's Archive for Clinical and Experimental Ophthalmology, revealed that eyes with inferior optic disc rotation had faster VF progression in the superior peripheral region, while those with superior optic disc rotation experienced more rapid decline in the inferior peripheral region.
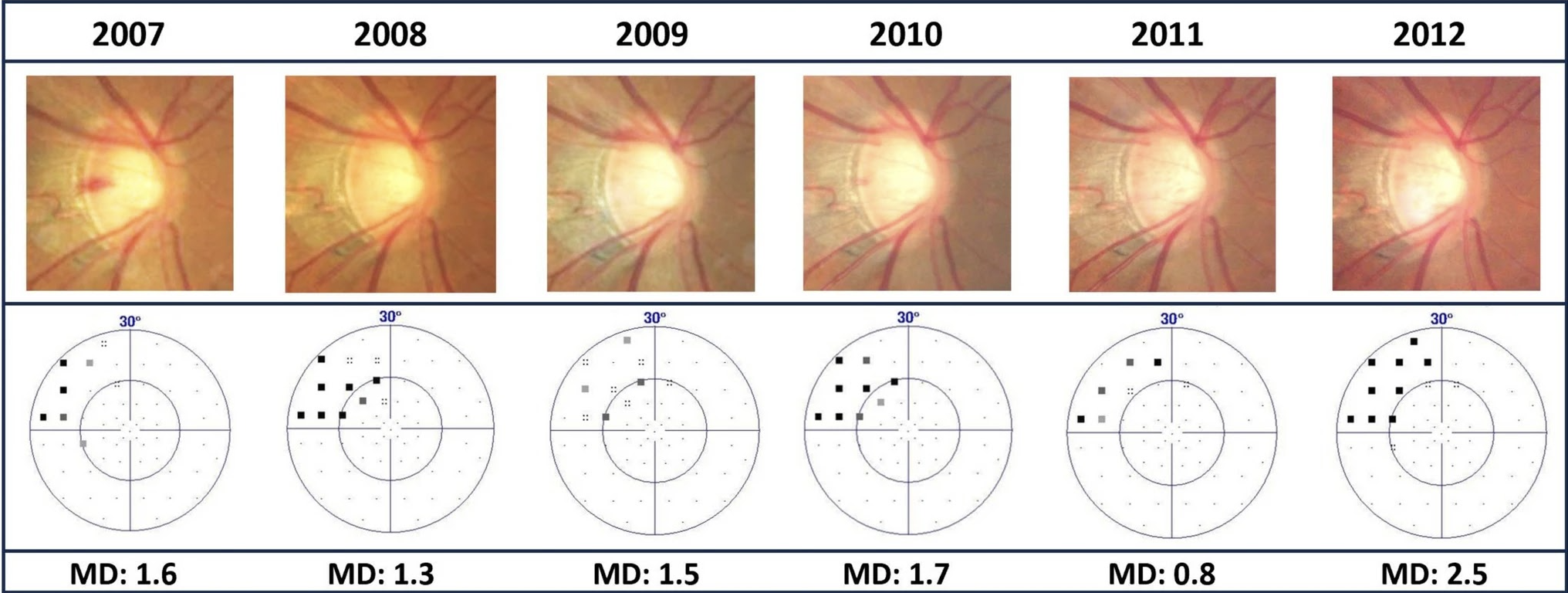 |
| In this study on patients with myopic open-angle glaucoma, cases of inferior disc rotation had the most considerable progression in the superior peripheral region and vice-versa. Photo: Tu P-N et al. Graefes Arch Clin Exp Ophthalmol. Dec. 27, 2024. Click image to enlarge. |
The researchers enlisted 53 myopic patients diagnosed with open-angle glaucoma. Thirty-two patients (60.4%) were male and the average age was 46.9 ±9.4 years. Over a three-year follow-up period, detailed ophthalmic examinations were performed including visual acuity and intraocular pressure measurements and eye imaging studies to assess optic disc rotation. The team performed statistical analyses of the data and reported the following findings:
69.8% of the studied eyes displayed inferior optic disc rotation
77.4% showed corresponding optic disc rotation and visual field defect.
a greater proportion of eyes (81.1%) in the inferior rotation group had initial superior hemifeld VF defect
the superior rotation group had a greater percentage of eyes (68.8%) with initial inferior hemifeld VF defect as well as significantly faster VF progression in the inferior peripheral region
The most notable correlation was between inferior optic disc rotation and more rapid visual field deterioration in the superior peripheral field, the researchers pointed out in their study. They offered one possible explanation: “The inferiorly rotated optic discs may indicate greater tensile stress at the inferior peripapillary scleral region,” they explained. “The vertically asymmetric mechanical stress on the lamina cribrosa and the stretching of the axonal fibers might weaken [both structures], which could lead to glaucomatous damage and corresponding superior VF defect.” Conversely, the authors noted that since “the superior optic nerve heads bear less burden in the inferiorly rotated optic discs, the superior lamina cribrosa and axonal fibers may not be affected by glaucomatous damage.”
Larger studies are still needed to confirm these observations. It’s also important to note, the researchers disclose in their paper, that all eyes included in this study had mild to moderate glaucoma; therefore, it remains unclear whether these findings extend to individuals suffering from severe glaucoma.
Nonetheless, the study authors conclude that their findings suggest “the clinical evaluation of the direction of optic disc rotation and optic disc rotation-VF defect correspondence may help clinicians manage patients with myopic OAG.”
| Click here for journal source. |
Tu PN, Hung CH, Chen YC. Implications of optic disc rotation in the visual field progression of myopic open-angle glaucoma. Graefes Arch Clin Exp Ophthalmol. December 27, 2024. [Epub ahead of print]. |



