 |
|
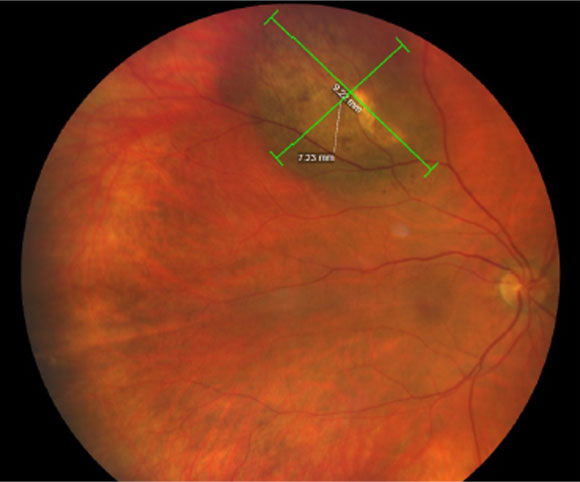
The authors discuss in their writing that many known risk factors like white race, light skin and eye color suggest an important role of UV light exposure in UM pathogenesis. Photo: Amy Bade, OD. Click image to enlarge. |
The most common primary intraocular cancer in adults is uveal melanoma (UM); however, it remains a relatively rare malignancy. Even rarer is its presentation in a younger population, thus currently attributing to the lack of risk factors specified for UM in adolescents and young adults. A retrospective study recently published in Ophthalmology Science addresses just this problem, analyzing demographics, genetic data, environmental exposures as well as social, medical and ocular history of UM patients to determine risk factors of younger populations.
Included in the investigation was a total of 247 UM patients aged 13 to 45 treated with proton beam radiation therapy and 401 age- and sex-matched controls. Median age at diagnosis was 38, with a median follow-up of 102 months.
Many novel risk factors were identified by the study authors, listed below with the odds ratio (OR) for each:
- family history of cutaneous melanoma (OR 3.06)
- Ashkenazi Jewish ancestry (OR 2.98)
- prior eye trauma (OR 2.94)
- secondhand cigarette smoke exposure (OR 2.39)
previous head and neck surgery (OR 1.81)
Along with these new observations, the present study also assessed established risk factors, too:
- choroidal nevi (OR 11.39)
- light eye color (OR 4.69)
- white race (OR 4.63)
- outdoor sunlight exposure (OR 4.20)
- recent pregnancy (OR 3.02)
- occupational and toxic exposures (OR 2.39 and 2.27, respectively)
- family history of any cancer (OR 2.16)
- lack of using ultraviolet-blocking eyewear (OR 2.13)
- indoor tanning (OR 2.10)
propensity to sunburn (OR 1.89)
It was found that oculodermal melanocytosis prevalence and UM in family history were significantly greater in this set of patients than controls. UM classification was small in 39%, medium-sized in 37%, large in 19% and very large in 5%. Three mutations of genes were identified from 13 patients who underwent germline genetic screening, with mutations in genes CDH1, NF1 and PALB2. However, the estimated 10-year metastasis-free progression rate and overall survival rates were better for this younger group than average adult populations, with rates of 80% and 81%, respectively, compared with the more general rates of 73% and 55%.
The authors further discuss some risks in their writing. Of interest was the novel finding of eye trauma. They note that there was no clinical difference seen in surveillance pattern for patients with prior eye trauma before diagnosis of UM. Because of this, “considering an increased chance of developing UM observed in our UM patients, obtaining a comprehensive ocular history is warranted at routine eye exams and initial ocular oncology evaluations,” the authors write.
They also explain that incidence of multiple primary malignancies was greater in this patient population (15%) vs. those of the general cancer population (2.4% to 8%). Because of the germline mutations seen in certain genes, which are often associated with hereditary malignancies, the authors also recommend “thorough characterization of the family cancer tree and genetic testing may be warranted in adolescents and young adults with newly diagnosed UMs to inform the necessity of screening for other malignancies.”
This leads them to the more general advice that, “given multiple risk factors that have been identified in association with UM, our study highlights the importance of obtaining a complete medical, social and family history as a risk assessment to evaluate all patients at risk for UM.”
| Click here for journal source. |
Nisanova A, Park SS, Amin A, et al. Novel risk factors for uveal melanoma in adolescent and young adult patients: a comprehensive case-controls analysis. Ophthalmol Sci. December 24, 2024. [Epub ahead of print]. |



