 |
|
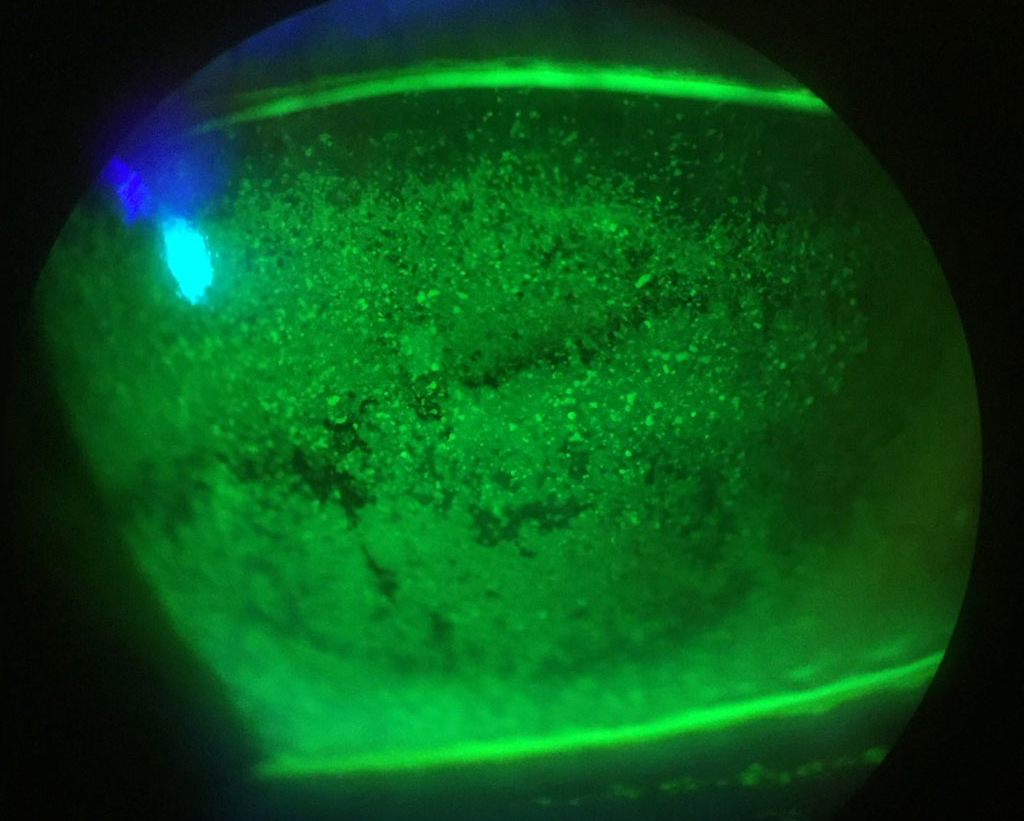
There remains great variability in clinical approaches to DED management worldwide. Until research evidence definitively improves guidance, data from this survey can be used by clinicians to benchmark their practice. Photo: Alexandra Wiechmann, OD. Click image to enlarge. |
It’s well known that the Tear Film and Ocular Surface Society (TFOS) 2nd Dry Eye Workshop (DEWS II) reports provide expert consensus recommendations for the diagnosis and management of dry eye disease (DED). However, there remains limited evidence to guide practitioners as to which treatment may be expected to be most effective for each DED severity and subtype. In a recent study, experts from TFOS relaunched the society’s international survey after five years to re-evaluate clinical dry eye prescribing and management patterns worldwide and examine how this has changed since the reporting of TFOS DEWS II, with the aim of improving patient care. Results were recently published in The Ocular Surface.
Survey responses encompassed a broad spectrum of clinicians from over 50 countries, across six continents, ranging from newly qualified to seasoned practitioners, likely the most wide-ranging survey of practitioners conducted to date. The content was chosen to reflect the management strategies reported by TFOS DEWS II. Questions were designed to ascertain practitioner treatment choice, depending on the subtype and severity of dry eye.
As was found in previous studies, the most commonly seen patients were those with mild symptoms and least common were those with severe symptoms. What the researchers found interesting was that practitioner experience had limited impact on the median severity or subtype over which different DED treatments were prescribed. However, the authors added, more experienced practitioners prescribed anti-inflammatory/immunosuppressants and secretagogues over a wider range of subtypes. “This was possibly due to confidence over their general effectiveness over time,” they wrote in their paper.
The most common treatment options were offering advice (82%) and recommending over-the-counter, low and high viscosity unpreserved lubricants and lid wipes/scrubs. “'Step 1' interventions in the TFOS DEWS II management algorithm include patient education/advice, dietary advice, artificial tears and warm compresses, as they are conventional, low risk and widely available management approaches suitable for early stage disease,” the authors wrote.
There was an increase in the preference for unpreserved artificial tears vs. preserved, with the ratio of prescriptions increasing from 1.3:1 in the 2018-19 survey to 1.5:1 in 2023-24. “This is supported by TFOS DEWS II guidance, which advises the use of preservative-free products where possible, and is facilitated by a wider range of unpreserved artificial tears having come to market in recent years,” the authors wrote.
A greater proportion of lid wipes/scrubs was made up by those developed specifically for Demodex, rather than those for general lid cleansing. There was also an increase in the use of commercial warm compresses over home-made alternatives such as heated washcloths which have been shown to rapidly fall below an effective temperature, to the point where this is now advised by the majority of practitioners, the authors added. Usage of mechanical spinning brush tools for lid hygiene increased, matching that of lid margin debridement, which was previously favored; however, therapeutic expression was still used by more practitioners.
Another change was seen with in-office treatments, such as intense pulsed light therapy and combined inner lid warming and massage devices. “Five years ago, a slightly greater proportion of practitioners were performing the latter, but this has reversed, and the balance is now 1.5 times in favor of light therapies,” the authors wrote.
Among prescription therapies, the global use of topical tacrolimus increased significantly relative to lifitegrast (1.9:1 in 2024 vs. 1.2:1 in 2019) and topical steroids (0.4:1 in 2023-24 vs. 0.2:1 in 2018-19). Therapeutic contact lenses were still used by more respondents than autologous/allogeneic serum and amniotic membrane, and a greater number of respondents reported performing surgical procedures rather than intraductal probing.
The major reported approaches for managing aqueous-deficient dry eye (ADDE) were punctal occlusion, therapeutic contact lenses and secretagogues. In contrast, the use of oral essential fatty acids, topical lipid-containing products, lid hygiene and lid warming were the preferred management choice for evaporative dry eye (EDE).
There was less artificial tear prescribing in Latin America, lesser use of lipid-based products outside Europe and Australia and fewer prescriptions for antibiotics in Europe and anti-inflammatories along with secretagogues in Europe and Australia. There were less intercontinental differences in prescribing according to subtype, with ointments used more for ADDE in Latin America, lid hygiene being used more for EDE in Asia and the Middle East, systemic antibiotics being used less commonly for evaporative type dry eye in Africa and topical anti-inflammatories and immunomodulators being used less frequently for EDE in North and Latin America.
| Click here for journal source. |
Wolffsohn JS, Semp DA, Dutta D, et al. Clinical practice patterns in the management of dry eye disease: a TFOS International survey 2023-4. Ocul Surf. December 23, 2024. [Epub ahead of print.] |



