 |
|
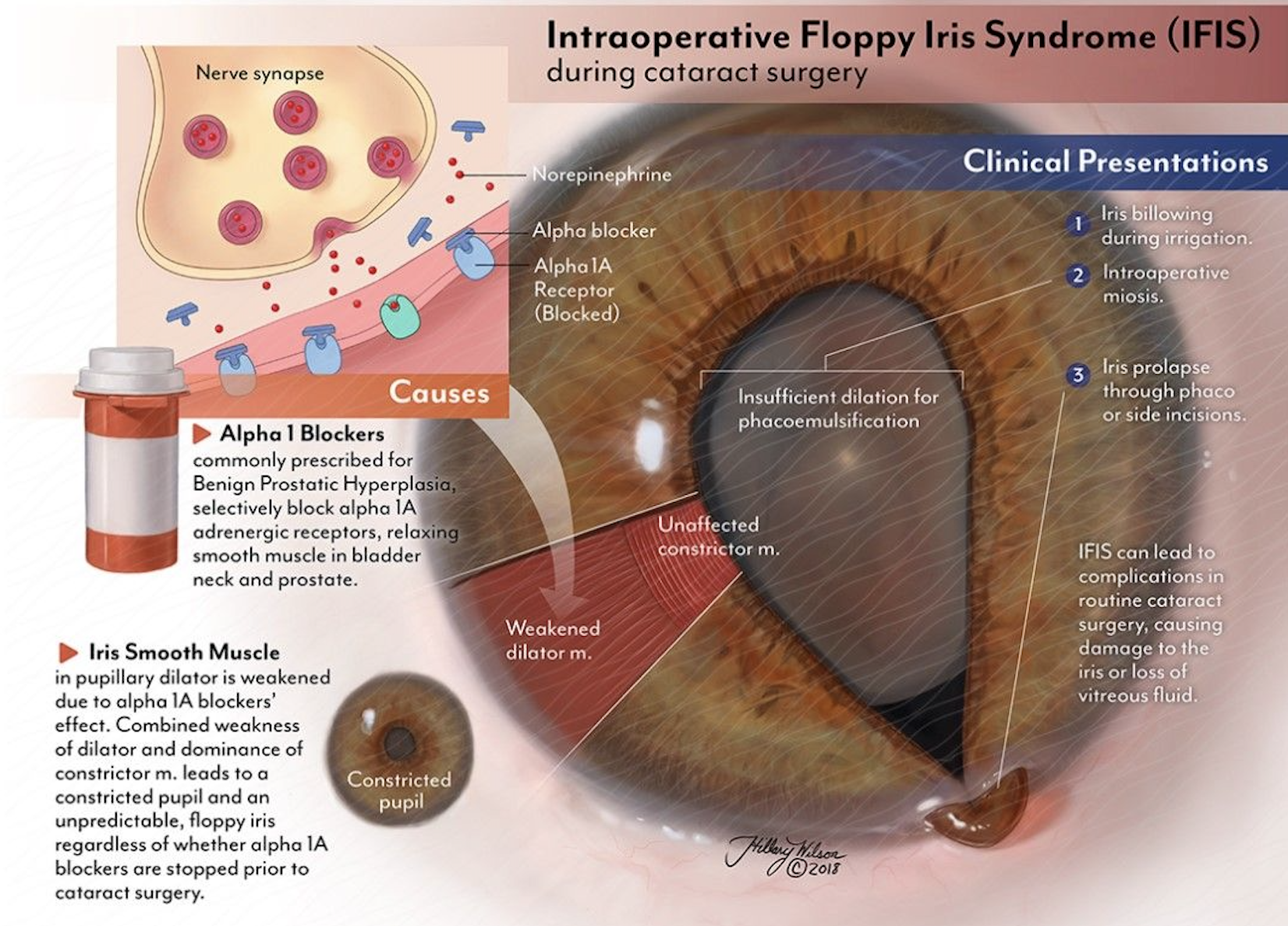
Three months of treatment with tamsulosin, often prescribed to patients with benign prostatic hyperplasia, was found to significantly reduce iris DMR thickness, DMR/SMR ratio, pre-dilation photopic pupil diameter and post-dilation pupil diameter. Since intraoperative floppy iris syndrome is more common among users of this medication, researchers advise monitoring iris thickness and pupil diameter changes before cataract surgery. Photo: Hillary Wilson. Click image to enlarge. |
Commonly used to treat benign prostatic hyperplasia, tamsulosin—an alpha-1 adrenergic receptor antagonist (α1-ARA)—has been linked with the cataract surgery complication intraoperative floppy iris syndrome.
Researchers hypothesize that the drug reduces iris dilator muscle thickness by blocking the alpha-1 adrenergic receptor. To investigate, a team of researchers conducted a prospective clinical before-and-after study that examined iris morphology, ciliary muscle thickness (CMT), pupil diameter and pupil responses to light in patients on this medication. They found that tamsulosin treatment led to a noticeable reduction in pre- and post-dilation iris dilator muscle region (DMR) thickness and the DMR to sphincter muscle region (SMR) ratio. Pupil diameter under photopic conditions also significantly reduced following treatment.
Forty-three patients with newly diagnosed benign prostatic hyperplasia were involved in the study. The following ocular parameters were measured before and three months after tamsulosin treatment using anterior segment OCT and corneal topography: iris DMR thickness, SMR thickness, DMR/SMR ratio, pupil diameter (scotopic, mesopic and photopic light conditions), CMT1 (1mm posterior to the scleral spur), CMT2 (2mm posterior to the scleral spur), CMT3 (3mm posterior to the scleral spur) and anterior chamber depth.
The results showed a reduction in the DMR thickness from 445.04±70.67µm before treatment to 384.41±84.40µm post-treatment. There was also a statistically significant decrease in the DMR to SMR ratio after tamsulosin treatment, indicating a relative change in the proportions of these muscle regions within the iris.
A notable decrease in photopic pupil diameter was also observed (from 3.26 to 3.12), while pupil size under mesopic and scotopic conditions was not significantly different after treatment; however, the study authors noted in their recent paper for American Journal of Ophthalmology that, “If the patients had been followed up for a longer period, the reduction in pupil diameter might have reached statistical significance in all light conditions.”
The following showed no significant differences after treatment: pre- and post-dilation iris SMR thickness, pre- and post-dilation CMT1, CMT2 and CMT3, pupil dilation speed and pre- and post-dilation anterior chamber depth.
“Tamsulosin potently and chronically antagonizes the α1a receptor on the iris dilator muscle in patients with benign prostatic hyperplasia,” the authors wrote in their study. “For this reason, tamsulosin may cause the loss of iris dilator muscle tone and disuse atrophy.” The team also provided a possible explanation for why CMT1, CMT2 and CMT3 values did not change after tamsulosin treatment, noting that since “tamsulosin is a weak antagonist of α1b adrenoreceptors, the thickness of the ciliary muscle may not have been affected.”
Additionally, the authors found a correlation between pupil diameter and the iris DMR and DMR/SMR ratio, hinting that “the reduction in DMR thickness resulting from the use of α1-ARAs can be effective in reducing pupil dilation.”
Since intraoperative floppy iris syndrome is more common among those taking α1-ARAs like tamsulosin, the researchers suggest “it may be necessary to take additional precautions during surgery in patients with iris thicknesses and pupil diameter measurements below a certain cutoff value.” Lastly, they advise, “Further studies with other α1-ARAs are required, as α1b receptors are more common in the ciliary muscle.”
| Click here for journal source. |
Öztürk C, Cevher S, Duran M, Ekici M. The effect of tamsulosin on iris morphology, ciliary muscle thickness, and pupil diameter. Am J Ophthalmol. December 16, 2024. [Epub ahead of print]. |



